by Lodi Vet | Aug 10, 2018 | Educational Materials, Equine
What is conjunctivitis and how do I recognize it?
Conjunctivitis is where the tissues surrounding the horse’s eyes become irritated by allergens, excessive dust, flies, injury, or a combination of irritants. The eyes appear red and watery and often the nasolacrimal (tear) duct becomes inflamed and swollen as well and no longer drains the eye normally.
Symptoms include:
- Inflammation of the mucous membrane or pink lining that surrounds the eyeball
- Redness of eye tissues
- Swelling and watering of eyes, sticky
- Yellowish discharge
- Often times refusal of horse to open the eyes or repeated clenching of eyelids
Conjunctivitis may be caused by any number of irritants, including dust, pollen, insect bites, flies, allergens, or it may also be the result of injury to the eye.
Unfortunately it is impossible to determine whether it is a simple form of conjunctivitis or if the conjunctivitis is accompanying a more serious condition such as a corneal ulcer so it should always be given immediate attention.
How can we treat it?
Removing known irritants from the environment is the first step in preventing conjunctivitis. Keeping dust of all kinds at a minimum, having an insect control plan in place, and taking care to prevent injuries to the horse’s eyes will help lessen the problem. In the case of ongoing or repeated cases of conjunctivitis a fly mask may be a large help in managing the problem.
In cases of simple conjunctivitis, merely removing the offending irritant can help solve the problem.
However in cases of more serious conjunctivitis it will be necessary to perform an examination of the cornea to be sure there are no corneal ulcers and then start the horse on an ophthalmic ointment with a steroid. The steroid works to decrease inflammation and calm down the irritated tissues. Since steroids decrease the eye’s ability to heal, it is imperative to be sure that there is no corneal ulcer present when you begin to administer the medication.
Equine ophthalmic issues can evolve from simple to serious very quickly so please do not hesitate to call your veterinarian if you have any questions or concerns regarding your horse’s eyes. We are open 24/7 for emergencies (608) 592-7755.
by Lodi Vet | Aug 9, 2018 | Cats, Dogs, How To
Physical Exam and Ear Swabs – WHY?
It is important to have an exam by the doctor and perform diagnostics (i.e. Ear Swabs) to determine the cause of the ear infection. The doctor must evaluate the ear drum to verify it is intact before prescribing ear medication, as some ear medications are toxic to the middle/inner ear. There are also different ear cleaners that are targeted to treat your pet’s specific ear condition. Once your veterinarian has prescribed the appropriate ear cleaner and medication you are ready to start.
Important Reminders
- Restraint: Restraint, depending on your dog or cat’s temperament, may be a two-person job (one person to restrain, another to clean).
- Cats: If you have someone available to help, have them hold the cat on a table cradled next to their body. Have the person hold the front lets and chest tight so the cat can’t get away. Use a towel to restrain if the cat is too wiggly. Wrap the cat up like you would if you were wrapping a burrito/taco. Be careful not to wrap too tight.
- Dogs: If you have someone available to help, have them hold the dog in a sitting-position between their legs facing you. It is often helpful to have the dog backed-up into a corner in the sitting-position to prevent the dog from backing out from the restrainer’s legs.
Cleaning
Note: Cleaning can be messy, so it should be done in an easy-to-clean area such as your kitchen or bathroom or even outside.
- Lift the ear pinna (ear flap) so you can see the opening to the ear canal.
- Fill the entire ear canal with your cleaning solution until you see the solution flowing out of the ear.
- Massage the ear canal. You will hear a “swish-swish” sound (like a washing machine). This action helps loosen the debris deep down in the ear canal.
- Stand back and let your pet shake its head. The shaking will push the loosened debris up and out of the ear canal.
- Wrap a piece of paper towel or Kleenex around your finger and gently blot out the excess debris and moisture. Don’t worry about pushing your finger too far into the canal. The ear canal is “L” shaped, so there is no threat of your finger reaching the ear drum.
Use caution when using q-tips to clean your pet’s ears. The q-tip is small enough that it could cause damage to the ear drum.
by Lodi Vet | May 31, 2018 | Educational Materials, Equine
The Buzz About EEE and WNV
There has been a recent resurgence in mosquito-borne diseases in Wisconsin over the last few years, and it has become even more vital that horse owners vaccinate against both Encephalitis and West Nile Virus. Last year, there were 24 cases of West Nile Virus (only 1 had been vaccinated) and 24 cases of Eastern Equine Encephalitis (only 1 horse had been vaccinated) in Wisconsin. Typically, when a horse contracts one of these diseases, it is due to not being vaccinated or being under vaccinated; thus, the goal of most equine practitioners is to ensure all horses are vaccinated and protected against these diseases.
Fun Fact: According to The Historical Medical Library of The College of Physicians of Philadelphia, horses and other animals were used to produce antitoxins in a variety of diseases, such as diphtheria, tetanus, and scarlet fever.
Recommended Vaccinations
The core vaccines recommended by AAEP are Eastern Equine Encephalitis (EEE), Western Equine Encephalitis (WEE), Tetanus, Rabies, and West Nile Virus. These vaccinations protect against diseases that occur year after year – by way of soil, insects or local wildlife; every horse is at risk, regardless of location or lifestyle. These vaccinations are safe, effective, widely available, and they prevent diseases that have a high mortality rate and/or no effective treatment. Additionally, the rabies vaccination helps protect human health and lives. Other vaccines may be recommended by your veterinarian depending on your horse’s specific needs/situation.
Who Can Vaccinate?
Vaccinations are available for over the counter purchase by anyone. However, it is strongly recommended that a veterinarian administer vaccines. If your horse was an adverse reaction associate with the vaccination or develops the disease while up-to-date on vaccines, the vaccine company will cover the cost of diagnostics and treatment when those vaccines were administered by a licensed veterinarian.
Vaccinating for Disease Prevention
Vaccination easily ranks as one of the single most important things you do to protect your horse’s health. Effectiveness of vaccines can be seen in human health history. Human diseases such as Smallpox and Polio have been almost 100% eradicated due to the use of vaccines; the last endemic case of Smallpox in the world occurred in Somalia in October 1977. While not all vaccines are as effective as these examples, most have significantly decreased the amount of disease.
Eastern Equine Encephalitis
A Brief History
The virus Eastern Equine Encephalomyelitis is thought to have been the case of EEE in North America since 1831. It did not receive its name until a major outbreak occurred in horses \in the coastal areas of Delaware, Maryland, New Jersey, and Virginia in 1933. Additional outbreaks occurred in Virginia and North Carolina in 1934 and 1935, respectively. Mosquitoes were first determined to be the carriers of EEE in 1934, and in 1950 it was discovered that birds can be a reservoir host for the virus.
Transmission
- Transmitted by mosquitoes or other biting insects
- Birds act as reservoirs for the virus; mosquitoes and other biting insects then carry the pathogen from infected birds and transmit it to horses when they bite
- The majority of wild birds infected with the virus will exhibit no clinical signs
- A horse affected with EEE is not contagious and poses no risk to other horses, humans or birds.
Incubation Period: 3-7 days
Carrier Status: Infected horses CANNOT transmit the disease to other horses, horses do not replicate enough virus to pass on to another mosquito
Severity: High; morbidity rate in horses infected with EEE is 75-95%
Clinical Signs
- Depression and anorexia without fever when initially infected
- Moderate to high fever 102.5-104.5F
- Lack of appetite, lethargy/drowsiness
- Neurologic signs- Onset of neurologic disease is frequently sudden and progressive
- Periods of hyperexcitability, apprehension and/or drowsiness
- Fine tremors and fasciculations of the face and neck muscle
- Convulsions
- Cranial nerve paralysis– facial paralysis and weakness of the tongue are very common
- Head tilt, droopy lip, muzzle deviation
- Weakness, ataxia, and dysmetria (incoordination) in one or all limbs o
- Complete paralysis of one or more limbs
- Colic
- Recumbency (inability to stand)
- Death
Diagnosis: Made by a veterinarian using combination of clinical signs, history and bloodwork
Treatment
- There is no cure for EEE
- Supportive care is administered in horses which show clinical signs
Prognosis
- Poor. Horses infected with EEE do not often survive
- Morbidity rate is 75-95% and death usually occurs within 2-3 days of onset of signs
Prevention
- Keep all horses up to date on vaccinations!
- Initial vaccination with booster, followed by yearly revaccination
- More frequent boosters (i.e. twice yearly) are recommended in areas with year-round mosquito seasons and in endemic areas
- Practice vector control management on your facility to reduce risk of transmission from insects.
- Use insect repellents frequently; re-apply after rain
- Keep horses in at night when possible, and apply insect repellent
- Eliminate or minimize standing water, eliminate brush piles, gutters, old tires and litter
- Remove all equipment in which standing water can collect
- Biosecurity: There are no recommended biosecurity protocols nor do restrictions need to be placed on affected or recovered animals as they pose no risk of infection to other horses.
West Nile Virus
WNV is a mosquito-borne virus that can cause encephalitis (inflammation of the brain) or meningitis (inflammation of the lining of the brain and spinal cord) in humans and horses. Mosquitoes acquire the virus from infected birds and transmit it to the dead end host In 1999, WNV was seen for the first time in New York. Since then, over 25,000 cases of WNV encephalitis have been reported in U.S. horses. Horses represent 96.9% of all reported non-human mammalian cases of WNV disease.
Transmission
- Transmitted by mosquitoes or other biting insects
- Birds act as reservoirs for the virus; mosquitoes and other biting insects then carry the pathogen from infected birds and transmit it to horses when they bite
- A horse affected with WNV encephalitis is not contagious and poses no risk to other horses, or birds
Incubation Period: 7-10 days
Carrier Status
- Infected horses CANNOT transmit the disease to other horses.
- The virus can only be transmitted to a horse via an insect vector
Severity: Medium. Up to 40% of infected horses are euthanized or die as a result of infection
Clinical Signs and Symptoms
- Depression and anorexia without fever when initially infected
- Mild low-grade fever (101.5-103.5F) in about 25% of affected horses
- Lack of appetite, lethargy/drowsiness
- Neurologic signs
- Paralysis
- Facial paralysis and weakness of the tongue are very common
- Recumbency (inability to stand)
- Incoordinationin one or more limbs
- Weakness
- Colic
- Death
Diagnosis
- Made by a veterinarian
- Use a combo of clinical signs, history and bloodwork
Treatment
- There is no cure for West Nile Virus
- Supportive care is administered in cases which show clinical signs
Prognosis
- Horses showing clinical signs of the disease develop in up to 39% of horses infected
- Some infected horses never show clinical signs of the disease and horses who survive usually make a full recovery
- Approximately 40% of horses will have residual neurologic deficits after recovering
- However, up to 40% of infected horses are euthanized or die if they become recumbent
References
- https://aaep.org/sites/default/files/Documents/Outside%20Linked%20Documents/DiseaseFactsheet_WNV.pdf
- https://aaep.org/sites/default/files/Documents/Outside%20Linked%20Documents/DiseaseFactsheet_EEE1.pdf
- https://equusmagazine.com/management/core-vaccines-25417
- https://www.aphis.usda.gov/publications/animal_health/content/printable_version/fs_eastern_equine_enceph.pdf
- https://cwhl.ahdc.vet.cornell.edu/disease/eastern-equine-encephalitis#collapse3
- https://extension.psu.edu/west-nile-virus-a-threat-to-horses
- https://www.vet.k-state.edu/vhc/services/equine/timely-topics/wnv-fact-sheet.pdf
- https://www.historyofvaccines.org/content/horse-serum
- http://www.equinediseasecc.org/disease-information
- https://aaep.org/guidelines/vaccination-guidelines
by Lodi Vet | May 25, 2018 | Educational Materials, Equine, Wellness
There are many poisonous plants in Wisconsin that could be a potential hazard to horses. These plants may cause symptoms such as:
- Colic
- Muscle weakness
- Incoordination
- Depression
- Paralysis
- Death
Undesired plants can be eliminated in pastures by several methods, however, hand pulling is often most effective. When eliminating these plants, be sure to:
- Wear gloves
- Pull plants up by the root (this is easier when the ground is wet)
- Dispose of the plants far from the horse’s reach
- Read instructions on any chemical herbicides thoroughly
- Keep animals off the area as directed after using herbicides
Below is a non-exhaustive list of commonly found plants that can be toxic to horses:
Black Locust
This tree can be found in almost every environment and soil. The bark, leaves, and seeds are all toxic.
- Symptoms: irregular heart rate, shallow breath, abdominal pain, and death
- Treatment: supportive care and detoxification
Black Walnut
While the tree itself is not toxic, shavings made from it and should not be used as horse bedding. Wilted or dry leaves can also be toxic for 4 weeks after falling from the tree.
- Symptoms: laminitis
- Treatment: treatment for laminitis
Bracken Fern
This plant is also known as Eastern Bracken. It is a perennial fern, and symptoms are slow to develop.
- Symptoms: depression, tremors, appetite loss, weakness, paralysis, staggering, loss of flesh
- Treatment: if caught in time, injections of thiamine can help reverse damage
Chokecherry
Chokecherry can be extremely lethal in small doses; as little as 2 pounds of leaves can kill an 800 pound animal in 30 minutes.
- Symptoms: convulsions, rapid breathing, frothing of the mouth, and dilated pupils
- Treatment: if caught in time, immediate supportive care and IV fluids, with an antidote of sodium nitrate and sodium thiosulfate
Cocklebur
Cockleburs are toxic when ingested. As little as 6 lbs. can be lethal to an 800 lbs. horse
- Symptoms: convulsions, depression, blindness, reluctance to move, hunched back, death
- Treatment: supportive care
Dried Maple Tree Leaves
While fresh leaves and twigs will not harm horses, wilted or dried leaves can be toxic.
- Symptoms: weakness, anemia, and increased respiratory rate
- Treatment: supportive care, IV fluids, blood transfusions and activated charcoal
Eastern Black Nightshade
This plant is also known as Deadly Nightshade, Horse Nettle, or Belladonna. It grows in hedges, pastures and in fence rows. It is a vine with purple flowers and green and red berries.
- Symptoms: depression, decreased heart and respiratory rate, muscle weakness, watery diarrhea, paralysis of hind legs
- Treatment: supportive care
Jimson Weed
This plant is also known as Devil’s Trumpet and Thorn Apple. As little as 1 lb. can cause symptoms and more can be fatal.
- Symptoms: dilated pupils, decreased respiratory rate, and muscle weakness
- Treatment: if caught in time, activated charcoal, supportive care, and IV fluids
Lawn Clippings
Lawn clippings become toxic as the grass ferments and releases a gas.
- Symptoms: gas colic
- Treatment: same as colic treatment
Oak Tree
The acorns, buds, leaves, and blossoms are toxic to horses and livestock.
- Symptoms: anorexia, colic, bloody diarrhea and edema
- Treatment: supportive care and IV fluids to flush out kidneys
Ornamental Yew
This plant is also known as Japanese Yew and is commonly used as a landscaping shrub. They are extremely toxic and as little as 6-8 ounces can kill a horse.
- Symptoms: weakness, labored breathing, collapse, trembling
- Treatment: if caught in time, treatment can include activated charcoal and assisted respiratory support
Rhododendron
This plant is also known as Mountain Laurel. It is extremely toxic to horses and as little as 0.2% of the body weight may be lethal.
- Symptoms: depression, weakness, impaired vision, difficulty breathing, collapse
- Treatment: if caught in time, treatment can include activated charcoal
Spotted Poison Hemlock
Also called Water Hemlock Cowbane, this plant is often found near creeks and streams in damp areas. As little as 2 pounds can cause death.
- Symptoms: incoordination, salivation, and colic
- Treatment: supportive care
White Snakeroot
This plant is often found along fence rows and woodlines.
- Symptoms: difficulty swallowing, muscle tremors, and wide stance
- Treatment: if caught in time, activated charcoal can be used
Images:
- https://wagwalking.com/horse/condition/black-locust-tree-poisoning
- https://csuvth.colostate.edu/poisonous_plants/Plants/Details/69
- http://noosasnativeplants.com.au/plants/414/pteridium-esculentum
- http://poisonousplants.ansci.cornell.edu/php/plants.php?action=indiv&byname=common&keynum=68
- https://www.fireflyforest.com/flowers/2542/xanthium-strumarium-rough-cocklebur/
- http://www.horsedvm.com/poisonous/red-maple/
- https://fyi.uwex.edu/weedsci/1993/10/04/1187/
- https://wagwalking.com/horse/condition/jimson-weed-poisoning
- http://www.herbalsafety.utep.edu/herbal-fact-sheets/jimsonweed/
- http://nwdistrict.ifas.ufl.edu/hort/2013/08/19/disposing-of-grass-clippings-can-be-a-pain-but-alternatives-exist/
- http://www.equestrianandhorse.com/care/pasture-grazing.html/poisonous-plants.html
- https://www.google.com/search?q=ornamental+yew&source=lnms&tbm=isch&sa=X&ved=0ahUKEwix98SJ66HbAhVs0YMKHYxnD_gQ_AUICygC&biw=906&bih=775#imgrc=LgIVDh4a4wzHGM:
- https://csuvth.colostate.edu/poisonous_plants/Plants/Details/111
- http://joshfecteau.com/poisonous-plants-spotted-water-hemlock/
- https://www.mnn.com/your-home/organic-farming-gardening/photos/13-plants-that-could-kill-you/white-snakeroot
by Lodi Vet | May 9, 2018 | Cats, Dogs, Educational Materials, Wellness
There are many changes that can occur in our pets as they age. These changes may require us to care for them differently than we may have when they were younger. This guide is intended to help you recognize the signs or symptoms common in our senior pets and ways to help them stay comfortable, safe and happy.
Decreased mobility
Mobility will decrease with time due to a combination of factors. Arthritis resulting in pain or decreased range of motion of the joints may cause difficulty in rising or laying down, or difficulty getting around. Muscle and nerve weakness can also lead to difficulty lifting the legs properly to walk — this may result in dragging or scuffing of the nails on the ground, or difficulty walking on slippery floors. Decreased mobility may result in your pet laying down most of the day — this can result in bed sores and infection or possibly swollen legs from decreased circulation from lack of movement.
Addressing lack of mobility will vary case to case depending on the severity and each pet’s particular needs. The following list are things that may help our pets with decreased mobility:
- Placing non-slip rugs, bath mats or yoga mats on slippery floors to provide traction.
- Trim excess hair that may be between toes that could reduce your pets natural traction.
- Move food and water bowls to a location where they can be easily accessed. For cats this means having the food on ground level so they do not have to jump up onto a counter, or walk down stairs to get to it.
- Use a litter box with lower edges to prevent need to climb or jump into the box
- Harnesses or slings can be used to help dogs stand from a laying position, or help them walk with our assistance. The Help Em Up Harness (www.helpemup.com) is a comfortable harness worn daily that has handles over the shoulders and hips that caretakers can use to help lift dogs into a standing position, or help them walk out to potty. Even a beach towel used like a sling could be helpful if your pet isn’t amenable to wearing a harness.
- Toe Grips – (www.toegrips.com) are non-slip nail grips that fit on a dog’s toenails to provide traction on slippery floors. They can be worn continuously, but will need to be replaced every 1-3 months.
- Use ramps to minimize number of steps a pet has to maneuver to go outside or into the car
- Medications — there are many safe and effective medications to treat arthritis pain.
- Acupuncture can be helpful in supporting nerve function and strength.
- Use of baby gates to protect pets from accidentally falling down stairs
- Comfortable bedding in a variety of areas to choose from
- Keep active — take small walks if tolerated to maintain muscle mass
Pain
Pain can come from many sources: arthritis, certain disease processes, decreased mobility. Speak with your veterinarian about signs of pain to watch for such as: heavy panting, pacing, whining, laying or sitting in an abnormal posture or location, or lack of appetite. There are safe and effective medications to treat the different types of pain our geriatric pets may experience. Laser therapy and acupuncture can be combined with traditional medications to help treat and control pain.
Hearing loss
By 8-10 years of age most of our pets will have some degree of hearing loss. This can pose safety concerns if they should become lost or if we need to call them away from a dangerous situation.
- Monitor your senior pet closely when outside, do not allow them outside alone if they are not contained in a fenced yard.
- Early on training your pets with both verbal and hand signals.
- It has been suggested that acupuncture can be helpful for age related hearing loss.
Decreased vision or blindness
Decreased vision or ability to see fine details is a common aging change. You may notice them missing treats on the floor or not being able to catch toys like they used to. Being able to see clearly at night is also a common complaint. Not all of our pets will completely lose their vision. If your pet suddenly becomes blind, a veterinary visit to evaluate vision and the eyes will be important in formulating a treatment plan. Ways to help our pets with decreased vision:
- Blocking off stairways using baby gates to prevent accidental falls
- Using night lights can help with decreased vision in poor lighting
- Not allowing pets with decreased vision outside alone to prevent accidents
- Use verbal commands or gentle touch to help guide them
- For pets who are blind the book “Living with Blind Dogs” by Caroline D. Levin can be very helpful
Incontinence
As muscles and nerves weaken with age, just as we see weakness in the hind legs, we can also see weakness in the muscles that control the bladder or rectum. This can result in urinary and/or fecal incontinence. Older pets may also have the urge to urinate or defecate more frequently. Hygiene can become an issue if they are urinating/defecating where they lay — this can lead to sores and infection. Depending on the severity of their incontinence, a variety of treatments are available:
- Medications can be used to help with urinary incontinence.
- Acupuncture may help improve continence
- Trimming hair near the urinary opening and anus and gently cleaning these areas with warm water on a rag to prevent sores/infection
- Use of Aquaphor ointment after cleaning near the urinary opening can reduce urine scald
- Sanitary napkins, belly bands and diapers can be used – these may increase risk of urinary tract infection.
- Covering their bedding with disposable absorbent pads (like puppy training pads or hospital chux)
- Working with your veterinarian to frequently monitor for urinary tract infections which become very common in our geriatric patients with incontinence.
- Having litter boxes with lower walls and in a variety of locations on every floor of the home for easy access
- Creating an indoor potty area for dogs to use “in an emergency” when you are away (using puppy pads, dog size litter pans, artificial turf, etc)
- Letting dogs outside to potty more frequently to reduce accidents inside
Appetite
Medical conditions that our geriatric pets may have can contribute to a decreased appetite. Nutrition is important for energy and maintaining weight.
- Appetite stimulants are available in a variety of forms
- Anti-nausea medications can be used in patients with diseases that may cause nausea (kidney disease, liver disease, pancreatitis, intestinal disease, etc.)
- Vitamin B12 injections are a natural appetite stimulant that may be of benefit
- Encourage appetite by feeding foods that are both enticing, but unlikely to cause gastrointestinal upset such as: cooked white rice, cooked noodles, boiled skinless potato, lean cooked protein, protein based baby food purees. Your veterinarian may have other recommendations based on your pets specific medical needs.
Hydration
Just as with food, some of our pets will become disinterested in drinking water. Hydration is very important for our pets, especially as they get older. Maintaining normal hydration can improve how our pets feel.
- Have multiple bowls of water around the house in easily accessible locations
- Use a pet water fountain — fresh running water can be more enticing
- Use low sodium chicken broth
- Try making low sodium chicken broth with gelatin added to create a “treat”
- Your veterinary team can teach you how to give fluid under the skin
Cognitive dysfunction
Behavioral changes can be some of the more concerning changes that occur in our older pets. Signs can include: aimlessly wandering or pacing the house, altered sleep/wake cycles, acting confused, getting lost in the house, not recognising familiar people or pets, regression in potty training or personality changes. It can be natural to want to scold them for making mistakes, or waking us at night, but we need to remember that these actions are usually not on purpose. Unfortunately there is no cure for cognitive dysfunction, several modalities have been tried with variable success rates. The following have been found to be helpful in some cases.
- Feeding a diet fortified with antioxidants
- Hill’s Prescription diet B/D (canine only)
- Purina ProPlan Veterinary Diets Neurocare (canine only)
- Anipryl (selegiline HCL) is a daily oral medication that can help reduce symptoms of cognitive dysfunction (can take up to 4 weeks to see a response) (canine only)
- S-Adenylmethionine is a daily chewable tablet that contains a powerful antioxidant which can be helpful in reduction in symptoms (canine and feline)
- Environmental enrichment such as regular exercise and introduction of new toys or rotation of toys can help stimulate the brain and slow progression of cognitive dysfunction
- Studies have shown that dogs that were given both dietary and environmental enrichment had the greatest improvement in cognitive dysfunction when compared to dogs who did not have enrichment.
Happiness
Of course this is the most important, but often overlooked, key to helping our geriatric pets. We love them unconditionally and because of this we, as pet owners, are the most important judge of their happiness. Keep in mind the things that make them special to you, what they love best, what gives them joy. Remember that even as the burden of caring for them increases with age we also need to keep in mind and provide them the things that bring them joy — whether it be car rides, walks (or trips outside in a wagon or stroller), a nap in the perfect sun spot, a visit with a special friend, beloved toys, favorite snacks, snuggles and cuddles with you.Caring for our pets as they age and develop medical conditions can be difficult. But we, at Lodi Veterinary Care understand the loving bond that connects us with our fur-children. If you have questions or concerns of the best ways or options to treat and help your pet, do not hesitate calling at any time.
by Lodi Vet | Apr 27, 2018 | Dogs, Educational Materials
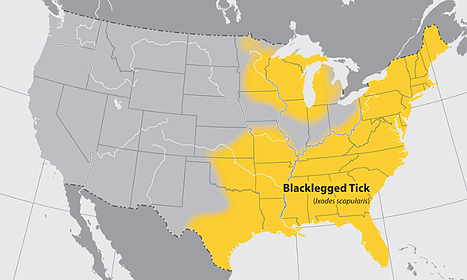
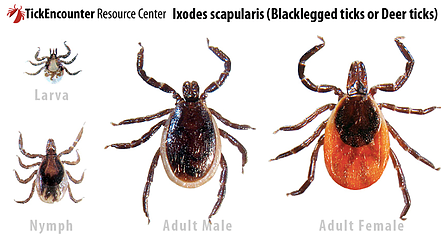
Anaplasma phagocytophila (formerly Ehrlichia equi) is a tick-borne disease which causes Equine Granulocytic Ehrlichiosis. This non-contagious disease is transmitted by the deer tick or blacklegged tick called Ixodes scapularis. (In western states it is also transmitted by Ixodes pacificus, the western blacklegged tick.) Small rodents such as white-footed mice, chipmunks, voles, and shrews, as well as white-tailed deer and possibly birds act as intermediate hosts in the lifecycle. Dogs, humans, and horses are incidental hosts.
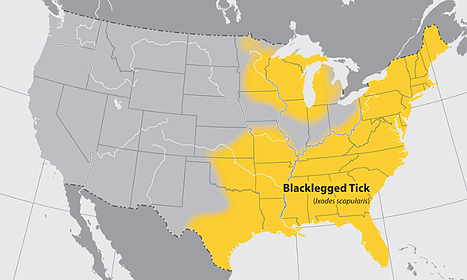
Image courtesy of cdc.gov
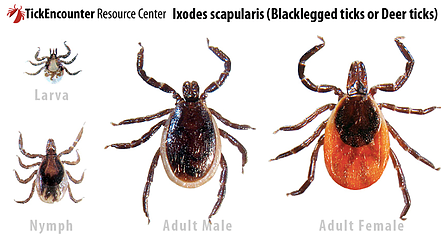
Image courtesy of the TickEncounter Resource Center
Any age or sex of horses can be affected, but horses younger than four years old seem to exhibit less severe signs.
Common signs may include:
-
Fever (often 103-106’F)
-
Colic
-
Decreased appetite
-
Limb swelling
-
Lethargy, unwillingness to move
-
Unsteadiness (ataxia)
-
Yellowish mucous membranes (icterus); may have small hemorrhages (petecchia)
-
Chronic infection: poor performance, change in attitude, lethargy, depression
-
Secondary problems may occur in horses with preexisting or concurrent problems
Diagnostic testing
There are several different testing options for anaplasmosis that involve bloodwork.
-
A blood smear may show inclusion bodies in white blood cells. Though very diagnostic, these are only present when the bacteria are reproducing.
-
A PCR is a send-out test which looks for DNA of the Anaplasma organism.
-
Other tests may include paired-titer levels, IFA test, or other depending on the situation.
Treatment may vary depending on the severity and other considerations, but generally would include a tetracycline antibiotic. Oxytetracycline administered intravenously once daily for about 5 days will generally result in a rapid and effective response. Doxycycline or minocycline given orally for a longer period can also be effective but typically has a much slower response rate. Horses undergoing treatment should be carefully monitored for side effects.
Non-steroidal anti-inflammatories (ex. Banamine) may also be used to help control fever.
Prevention:
No vaccine is currently available. At this time, the best prevention is targeted towards multifactorial tick control. Many products, such as tick leg bands and UltraBoss, can be used. In addition, environmental control is very important and may include keeping pastures mowed, trees pruned, and leaf litter to a minimum. It also helps to keep horses tails shorter than grass height and to decrease secondary hosts such as mice and shrews.
If you have any questions regarding the above information or your horse is displaying any of the signs listed above, please call us at (608)592-7755, we would be happy to discuss further.