by Lodi Vet | Sep 24, 2018 | Cats, Educational Materials
 Diabetes mellitus is a common problem in cats. Caring for a diabetic animal requires some effort, but most pets remain happy and comfortable. Successful patient management requires a team effort between you and our veterinary care team.
Diabetes mellitus is a common problem in cats. Caring for a diabetic animal requires some effort, but most pets remain happy and comfortable. Successful patient management requires a team effort between you and our veterinary care team.
What is diabetes mellitus?
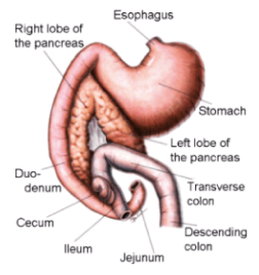
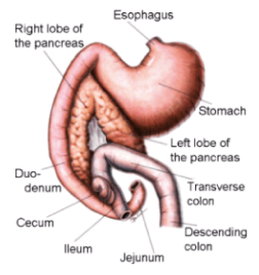
Diabetes mellitus is a disease caused by a deficiency of (or lack of response to) insulin. Insulin is a hormone that is produced by the pancreas. The cells of the body require blood sugar (glucose) for food and they depend on the bloodstream to bring glucose to them. The cells cannot, however, absorb and utilize glucose without insulin. Insulin is necessary for the movement of glucose from the blood into the cells of the body.
What are the signs of diabetes?
Excessive thirst, frequent urination, increased hunger, sudden weight loss and weakness are seen in cats with diabetes. Without insulin, glucose remains in the bloodstream and eventually passes into the urine. This causes increased urination, which then leads to an increase in thirst. Hunger increases because the body cannot use the glucose in the blood, which results in the body destroying muscle and fat to use as energy sources. If left untreated, this disease sets off a series of events which results in weight loss, major organ system failure, and eventually coma and death.
Why is my cat diabetic?
Feline diabetes is a complex disease, and most likely genetic and environmental factors both play a role. Many cats with diabetes have a history of chronic pancreatitis, or a disease which affects the body’s response to insulin. We do know that obesity is commonly associated with feline diabetes, along with the use of certain medications, such as steroids.
Is there a cure for diabetes?
Although there is currently no cure for cats with diabetes, some cats undergo remission a few months after diagnosis. This means that the diabetes goes away temporarily, and the cat is once again able to control his or her blood glucose levels. There is evidence to suggest that remission is most likely if the diabetes is treated effectively when first diagnosed.
How is diabetes treated?
Treatment generally requires an injection of insulin under the skin twice daily. Successful treatment also involves a high protein, low carbohydrate diet, generally Hill’s m/d or Purina DM.
What does the insulin do?
Insulin moves glucose from the blood into the cells. Glucose is an essential fuel for most of the tissues in the body, and without insulin, cell metabolism is severely compromised. Providing insulin in the form of an injection allows your cat to be able to utilize its glucose and maintain relatively normal glucose levels.
How do I give insulin?
Our veterinary team will show you exactly how to give insulin injections, but it’s really very simple. The insulin dose it pulled up into a special syringe, and injected under the skin. It is often easiest to inject between the shoulder blades or along the neck.
Do the insulin injections hurt?
Insulin syringes have very small needles, and most cats do not notice the injection. It is often easiest to administer the injection while your cat is distracted with food, a treat, or a toy. Most people are surprised at how easy insulin injections are to give.
How do I dispose of my used supply of needles and syringes?
Used needles and syringes need to be properly disposed of for both your safety and ours. You will be required to purchase a “SHARPS” container for a fee. This fee covers the container purchase, plus the proper disposal of the used/full container.
We will not accept used needles and syringes that are stored in containers other than the approved “SHARPS” container. Once the “SHARPS” container is full, simply return it to our office. We will dispose of it and you can purchase a replacement container.
What follow-up is involved with treating diabetes in cats?
In the non-diabetic cat, adequate amounts of insulin are produced continually (or as needed) by the pancreas to maintain normal blood sugar levels. When we give insulin injections, we administer a fixed amount at one time and that insulin is slowly released over several hours. A blood glucose curve is needed to determine how fast the injected insulin gets into the bloodstream and how long it lasts. Based on these results, we can determine if the correct type of insulin is being used and if the dose needs to be adjusted. Blood glucose curves are needed periodically to insure that the proper amount of insulin is being used. Blood glucose curves are performed by obtaining a blood glucose level every 2-4 hours over a 12 hour period. Generally, if your cat’s blood glucose is elevated throughout the curve, their insulin dose needs to be increased. If your cat’s blood glucose level is too low throughout or at any point during the curve, the insulin dose needs to be decreased.
What are the possible complications associated with treating my cat with insulin?
The most serious complication involved in treatment of diabetes is administration of too much insulin, which can trigger a dramatic drop in blood sugar leading to weakness, nausea, incoordination, seizures, and even death. Immediate feeding of a sugary food (honey, syrup, etc.) usually helps reverse this reaction. Other difficulties encountered generally revolve around finding the correct amount, timing and type of insulin given. While this is not often the case, “problem diabetics” do exist and have a higher incidence of concurrent disease such as lower urinary tract infections, kidney disease and liver disease.
Can I monitor my cat’s blood sugar (glucose) at home?
Learning to measure your cat’s glucose levels is very worthwhile. Firstly, information collected at home is a reflection of what’s happening day to day in your cat’s normal living environment. Cats in particular can become very stressed in the clinic, and their blood sugar levels can become markedly increased. Home glucose monitoring would allow you to be able to perform your cat’s glucose curves at home. Our veterinary team can use the values you obtain at home to adjust insulin therapy more appropriately and accurately. Secondly, if your cat seems unwell, you can quickly determine if blood sugar levels are dangerously high or low. It is very important to always consult our veterinary team prior to making any insulin adjustments.
The thought of glucose home monitoring may seem overwhelming at first, but it is an option to consider and can be started at any time during your cat’s diabetic treatment. Our veterinary team would be happy to demonstrate proper and easy blood sampling techniques and provide a home glucose monitoring kit.
What are the costs associated with treating my diabetic cat?
The major costs associated with treatment of diabetes include insulin, syringes and the cost of the glucose curves to regulate insulin requirements. We can give you more accurate estimation of treatment cost at your consultation appointment.
Our veterinary care team has reviewed the following websites on feline diabetes and find them to be an accurate source of valuable information.
www.veterinarypartner.com
www.alphatrakmeter.com
Making the decision to care for your cat with diabetes is a big commitment, but many owners of diabetic cats have found treatment to be a very rewarding and enriching experience. There is a lot to learn and it is important to be patient with yourself and your cat during the learning process. Diabetes is a serious disease, but it can usually be well-controlled, enabling your pet to lead a happy and comfortable life.
by Lodi Vet | Sep 23, 2018 | Dogs, Educational Materials
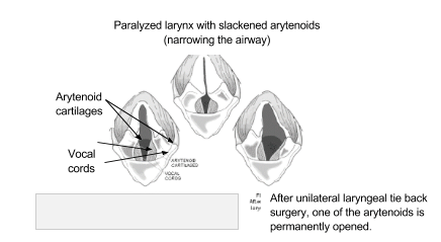
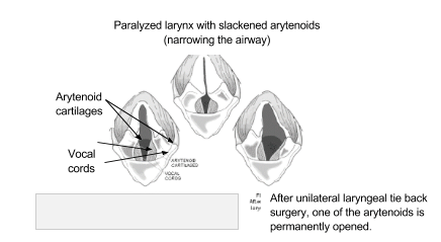
The larynx (or voice box) is a structure located in the throat that helps direct air into the lungs and food into the esophagus. Its function is important in preventing food/water from entering the lower airways when swallowing. The larynx opening and closing is controlled by two small flaps called the arytenoids – these arytenoids close when we swallow food/water and open when we take a breath.
Laryngeal paralysis is when the nerves to one or both of the arytenoids become weakened or stop working entirely. This results in one or both of the flaps controlling the larynx to become paralyzed causing them to become slack. This causes louder raspy noise while breathing caused by the slackened arytenoids vibrating as air flows past them. Because of this weakening dogs can inadvertently swallow food or water into the lower airways resulting in coughing or even pneumonia.
The exact cause of laryngeal paralysis is yet unknown. It has been found that dogs with hypothyroidism are more prone to laryngeal paralysis. One study suggests that laryngeal paralysis may be part of a more widespread nerve degeneration; often times dogs with laryngeal paralysis also have weakness in the hind limbs.
Diagnosis of laryngeal paralysis is made by observation of the movement of the arytenoids as deep breaths are taken. This type of exam requires sedation. If one or both of the arytenoids appear slack the diagnosis is made. Occasionally chest x rays and bloodwork are also needed to better understand the situation.
Treatment of laryngeal paralysis is a surgical procedure called a laryngeal tie back or lateralization surgery. This surgery involves placing sutures to help reposition one of the arytenoids to open the airway. Unfortunately this surgery can present risks. Approximately 30% of dogs receiving this surgery will experience a complication called aspiration pneumonia in which food or water is swallowed into the lungs causing infection. Acute respiratory distress is another common complication of the surgery in which a patient will have difficulty breathing and may require an emergency tracheostomy to be placed (this is when a small hole is cut into the trachea below the surgery site to place a breathing tube).
If laryngeal paralysis is not treated the risk of respiratory crisis can occur. If a dog with laryngeal paralysis gets excited or is exposed to warm temperatures, they will begin to pant. Panting will cause the slackened arytenoids to hit each other repeatedly resulting in potentially life threatening swelling of the throat that could result in overheating, lack of oxygen to the brain, and/or death.
Helpful tips for dogs with laryngeal paralysis:
- Avoid stress to prevent excess panting
- Keep pet in a temperature controlled, cool environment avoiding extreme heat
- Use a harness instead of a collar to reduce pressure on the neck
- Ask your veterinarian if anti-inflammatory or anti-anxiety medications could be helpful
- Pursue surgical correction in a timely fashion to reduce risk of respiratory crisis
by Lodi Vet | Sep 23, 2018 | Dogs, Educational Materials
The vestibular system is a combination of sensing receptors in the middle ear which help us determine our orientation and movement. These receptors then send signals via nerves to parts of the brain that help us maintain balance and coordinate our movements. If any part of this intricate system is disrupted it can result in “vestibular disease”.
Symptoms of vestibular disease include: head tilt, ataxia or uncoordinated movements, walking in circles, falling over, motion sickness or nausea, and nystagmus (rapid eye movements side to side or rotational).
Causes of Vestibular Disease
- Middle ear infections can affect the vestibular organs which reside in the ear. Diagnosis can occasionally be made by external ear exam and microscopic evaluation of debris, but may require x rays of the bulla (bones of the inner ear). Treatment will involve topical and/or oral antibiotics. In severe cases, anesthesia for a deep ear flush may be warranted.
- Brain lesions such as cancer, bleeding or blood clots in or around the brain can be an important but less likely cause of vestibular symptoms. Diagnosis of this would require referral for CT scan or MRI.
- Idiopathic or “old dog vestibular disease” is the most common cause. Idiopathic disease has no known cause, but it occurs acutely and resolves quickly. Often dogs with this form will be back to normal in 7-14 days. Treatment involves treating for motion sickness and nausea. Physical therapy can also be helpful in assisting in recovery.
by Lodi Vet | Sep 23, 2018 | Cats, Dogs, Educational Materials
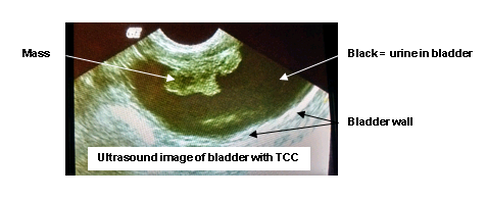
Transitional Cell Carcinoma (TCC) is a cancer of the urinary bladder. Transitional cells are the cells that line the bladder wall, TCC is a cancer that arises from these cells. The exact cause is unknown, however, an increased risk of this cancer is found in certain breeds of dogs. Shetland sheepdogs, West highland terriers, Scottish terriers and Beagles are breeds predisposed to TCC.
Symptoms include:
- Blood in the urine
- Straining to urinate
- Frequent or unexplained bladder infections
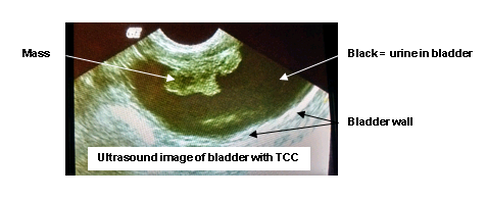
The diagnosis of TCC is often made after ruling out more common causes of the above list of symptoms (such as bladder stones, infections or other benign causes of blood in the urine and straining to urinate). Several diagnostic tests will be needed to confirm the diagnosis of TCC.
- Urinalysis – will reveal blood and sometimes abnormal cancer cells can be seen.
- Urine culture – allows for infection secondary to the tumors to be treated with appropriate antibiotics.
- Radiographs – rules out stones in the bladder
- Ultrasound – will show abnormal masses in the bladder wall, but can also show us crystals, stones or polyps in the bladder
- Cystoscopy – A tiny flexible camera that can be inserted like a catheter through the urethra into the bladder to help visualize and biopsy bladder masses
- Catheterization – in some cases a urinary catheter can be placed in male dogs that helps collect a small sample of cells for cytology
- Cytology — evaluation of cells by a pathologist
Treatment
- Chemotherapy – available through veterinary oncologists.
- Surgical removal – possible only if mass is in a location favorable for surgery.
- Conservative/palliative care – piroxicam is an oral medication often used due to its anti-inflammatory properties and possible anti-tumor activity.
Your veterinarian will help formulate a diagnosis and treatment plan best suited for your pet’s needs.
by Lodi Vet | Sep 23, 2018 | Dogs, Educational Materials
Keratoconjunctivitis sicca, otherwise known as KCS or Dry Eye is a condition in which tear production is abnormally low.
Symptoms may include one or more of the following:
- Dry appearance to the eye
- Increased thick ocular discharge
- Conjunctivitis – red/inflamed eyes
- Corneal edema (hazy white appearance to outer eye)
- Corneal pigmentation (brown discoloration to the outer eye)
Corneal ulcers or damage to outer eye can occur secondary to KCS
Diagnosis is made by performing a test to measure tear production called a Schirmer Tear Test. A fluorescein stain may be performed to help rule out corneal damage or ulceration secondary to KCS.
Treatment of KCS is life long and involves using a combination of therapies to help stimulate natural tear production, provide lubrication to the eye and control secondary bacterial infections. The most common medication used is an ophthalmic ointment called Optimmune (or other cyclosporine eye medications) – this treatment can stimulate tear production as well as decrease inflammation. Prognosis is good for patients with KCS, however treatment is lifelong.
by Lodi Vet | Sep 21, 2018 | Cats, Dogs, Educational Materials, Wellness
How to Look for Fleas on Your Pet
Examine your pet’s coat carefully. Using a fine-toothed comb (flea comb), look for adult fleas, or for specks that look like pepper (flea dirt). The most common areas to find fleas/flea dirt are the groin, armpits, tailhead, and the neck area. Transfer the black specks onto a white paper towel, and moisten it with water. If the specks leave a red stain, these are definatley flea droppings.
Flea Allergy Dermatitis
Many dogs and cats are allergic to flea saliva, and even a few bites cause these pets to be intensely ithcy. For these pets, flea prevention is critical. The skin irritation associated with flea bites can be treated with anti-inflammatories, and skin infections can be controlled with antibiotics.
Successful Flea Control
An effective flea control program requires treatment of all:
- Pets in the household
- Stages of fleas
- Areas of the environment
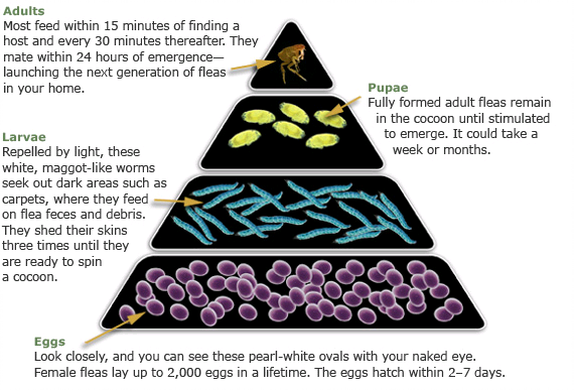
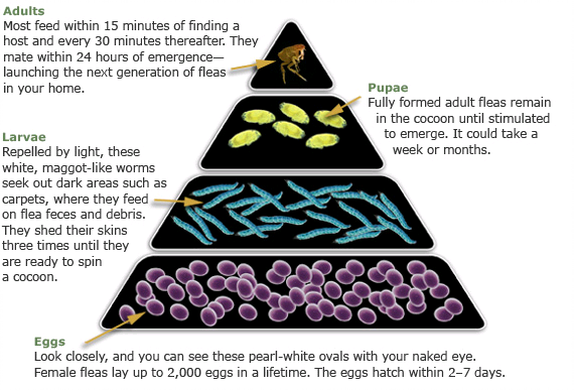
It is very important to use a flea control product that controls the larva and egg stages, as these stages comprise 95% of the flea population. Look for house treatments that contain insect growth regulators (IGRs) for effective control of all stages. Adult fleas spend a majority of their lives on a dog or cat, and are easily killed with an effective adulticide product.
Fleas complete their life cycles best in carpet/upholstry fibers, cracks or crevices on the floor, and in shady areas of yards. Concentrate control efforts in these areas. Prevention is easier and less costly than treating a flea infestation.
A. Treat the pet.
Adult fleas that are living on the pet must be killed. Effective products will not only treat an active infestation, they will prevent future infestations. It is recommended to use monthly.
These products include:
- Simparica – once monthly oral tablet for dogs only
- Comfortis – once monthly oral tablet for dogs and cats
- Parastar Plus – topical for dogs only
- Easy Spot – topical for cats only
- Revolution – topical
For pets with a significant amounts of flea dirt, we recommend administering product, waiting two (2) days, then bathe with an aloe/oatmeal shampoo. It is not recommended to use medicated shampoos or flea shampoos in conjunction with other products. These shampoos will strip, or remove, the topical products.
B. Treat the house/outdoor environment.
Remember that only 5% of the flea populations are adult fleas on the pet. The remaining 95% of the population are eggs, larvae, and pupae living in carpet and upholstery.
The recommended home treatment is a product called Knockout Spray (with IGR). One (1) can treats approximately 1200 – 1500 square feet.
Pre-treatment:
- Vacuum all carpets, upholstered furniture, baseboards, and under furniture. Discard vacuum cleaner bag immediately.
- Mop floors with warm, soapy water.
- Change all linens, blankets, and replace (or wash in hot water) pet bedding.
Treatment:
- Follow the directions on the can. All pets and humans must be out of the treated areas as directed on the can.
- Spray all carpeted areas and upholstery with the house treatment spray. Be sure to treat under furniture, and to treat all rooms in the house.
- If you pet spends a lot of time outside or in a kennel, these areas must be treated for fleas as well. Concentrate on shady, protected areas, and dog houses. Treat the areas according to label directions.
Follow-up treatment:
Repeating home treatment is very important. Fleas in the pupal stage are protected by the cocoon, therefore retreat in two (2) weeks to kill fleas that emerge.
C. Prevention
If your pet is exposed to other animals or are outside, they may become infested with fleas repeatedly. Consistent use of monthly preventatives is advised yearround to keep your pet protected from re-infestation.
- Simparica (dogs only): Give once monthly for control of fleas and ticks in dogs. Simparica has the advantage of being unaffected by swimming and bathing. Also, no residue on skin like other topical products.
- Parastar Plus (dogs only): Apply topically once a month for control of fleas and ticks in dogs. Water resistant
- Easy Spot (cats only): Apply topically once a month for flea and tick control in cats.
- Revolution: This product prevents heartworm disease, ear mites, sarcoptic mange, roundworms and hookworms, as well as fleas and ticks.
 Diabetes mellitus is a common problem in cats. Caring for a diabetic animal requires some effort, but most pets remain happy and comfortable. Successful patient management requires a team effort between you and our veterinary care team.
Diabetes mellitus is a common problem in cats. Caring for a diabetic animal requires some effort, but most pets remain happy and comfortable. Successful patient management requires a team effort between you and our veterinary care team.