We can all agree that the health of our horses is of the utmost importance to us. They are vulnerable to a number of transmissible diseases that can spread easily between horses. These diseases can cause a variety of symptoms, including respiratory signs, diarrhea, or...
Educational Materials
Colic – What does the vet mean?
Colic is a very broad term, describing signs of abdominal pain in the horse. If you are somewhat unsure of what colic truly means, you are certainly not alone! Colic has a number of different causes, and each cause of colic comes with varying treatment options, and...
Your Horse’s First Aid Kit
Do you have a first aid kit prepared for your horses? While a first aid kit is not meant to substitute veterinary care, it can be incredibly helpful in emergencies to help stabilize your horse until the vet can attend. Your kit will include essential equipment, as...
Why your veterinarian should be the one vaccinating your horses
When it comes to the safety and health of your four-legged companions, vaccination is an area where we don’t want to make compromises! Many of the diseases we routinely vaccinate for are very serious, if not fatal for your horse. Having a veterinarian vaccinate your...
Bull Breeding Soundness Exam
Spring is fast approaching and the breeding season is right around the corner. In order to ensure a successful breeding season, a bull breeding soundness exam (BSE) is essential. Most bulls are capable of breeding cows, however, some may be “sub-fertile” resulting in...
Don’t Let Your Herd Take a Step Backwards Due to Lameness
Most beef cows in the U.S. never see a hoof trimmer, nor do they need one. Our beef cows have been naturally selected for great feet and legs and don’t require much maintenance. Cattle on pasture have the ideal substrate to walk on: forgiving topsoil with adequate...
ProHeart 12 for heartworm disease prevention
One Dose. Once a Year. LVC is proud to now offer ProHeart 12 to our patients as a new option for heartworm prevention! ProHeart 12 is the only once-yearly injection to prevent heartworm disease and intestinal parasites in dogs. Heartworm disease is on the rise in...
Beef Cow Fall Program
Fall is an important time in the management of beef cows. Valuable management can include pregnancy exams, vaccinations, deworming and delousing. Pregnancy exams done in the fall can determine whether or not a cow is bred. Early determination of open cows can have a...
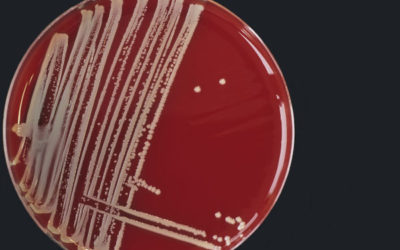
Mastitis Culture Aids in Treatment and Prevention Strategies
In recent years, the dairy industry has enjoyed steady improvements in milking equipment, cow environment, teat dips and genetics. While these improvements are notable, dairy producers are still faced with udder health challenges that range from fine tuning somatic...
Septic Arthritis in Cattle
Septic arthritis (commonly known as joint infections) are common in all breeds of cattle and can be life threatening to the animal. They are most commonly seen in young calves as secondary infections to umbilical (navel) infections shortly after birth. They may also...