Spring is fast approaching and the breeding season is right around the corner. In order to ensure a successful breeding season, a bull breeding soundness exam (BSE) is essential. Most bulls are capable of breeding cows, however, some may be “sub-fertile” resulting in...
Livestock
Don’t Let Your Herd Take a Step Backwards Due to Lameness
Most beef cows in the U.S. never see a hoof trimmer, nor do they need one. Our beef cows have been naturally selected for great feet and legs and don’t require much maintenance. Cattle on pasture have the ideal substrate to walk on: forgiving topsoil with adequate...
Beef Cow Fall Program
Fall is an important time in the management of beef cows. Valuable management can include pregnancy exams, vaccinations, deworming and delousing. Pregnancy exams done in the fall can determine whether or not a cow is bred. Early determination of open cows can have a...
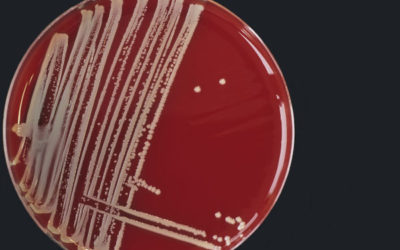
Mastitis Culture Aids in Treatment and Prevention Strategies
In recent years, the dairy industry has enjoyed steady improvements in milking equipment, cow environment, teat dips and genetics. While these improvements are notable, dairy producers are still faced with udder health challenges that range from fine tuning somatic...
Septic Arthritis in Cattle
Septic arthritis (commonly known as joint infections) are common in all breeds of cattle and can be life threatening to the animal. They are most commonly seen in young calves as secondary infections to umbilical (navel) infections shortly after birth. They may also...
LVC introduces a new procedure… Artificial Insemination and Embryo Transfer In Sheep and Goats
The advanced reproduction team at Lodi Veterinary Care is excited to announce Laparoscopic Artificial Insemination (AI) and Embryo Transfer (ET) procedures in sheep and goats. The laparoscopic AI procedure requires the animal to be lightly sedated, given a local block...
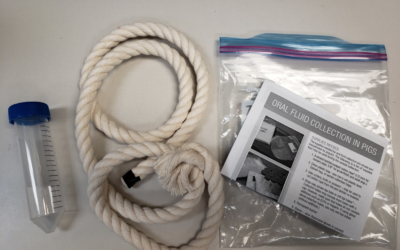
What You Need to Know Before Taking Your Pig to the Fair
Porcine Reproductive and Respiratory Syndrome (PRRS) and Porcine Epidemic Diarrhea Virus (PEDv) are common diseases present in pig populations. PRRS is a viral respiratory and reproductive disease which causes abortions and infertility in adult sows. PEDv is a virus...
Managing Calf Scours
Scours, or diarrhea, is a common illness of young calves and one of the leading causes of mortality prior to weaning. Affected calves may suffer from decreased appetite, weakness, and eventual death from dehydration or electrolyte imbalances. Fortunately, scours can...
The contagious truth about ringworm – let’s keep it out of our county fairs!
What is Ringworm? Ringworm is a common fungal infection of livestock that is caused by several different organisms called dermatophytes. The most common type to affect cattle is called Trichophyton verrucosum. How is ringworm transmitted? The organisms that cause...
A Different Breed of Pinkeye Emerges… Is a Different Breed of Vaccine the Answer?
What is pinkeye? Pinkeye is a very painful and bothersome disease of cattle that has changed greatly in recent years. Traditional pinkeye (Moraxella bovis) is a summertime, pasture-based problem, easily treated with antibiotics. Modern pinkeye (Moraxella bovoculi ) is...