One Dose. Once a Year. LVC is proud to now offer ProHeart 12 to our patients as a new option for heartworm prevention! ProHeart 12 is the only once-yearly injection to prevent heartworm disease and intestinal parasites in dogs. Heartworm disease is on the rise in...
Wellness
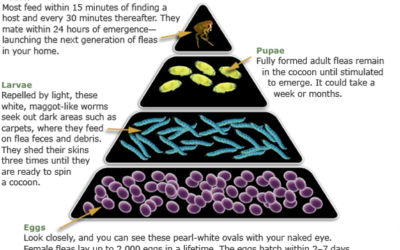
Flea Control Guide
How to Look for Fleas on Your Pet Examine your pet's coat carefully. Using a fine-toothed comb (flea comb), look for adult fleas, or for specks that look like pepper (flea dirt). The most common areas to find fleas/flea dirt are the groin, armpits, tailhead, and the...
What is a Coggins Anyway?
What is a Coggins Test? A coggins is a test for equine infectious anemia (EIA) which is a viral disease. Facts about EIA EIA is spread by blood-feeding insects such as horseflies, stable flies , and deer flies. It can also be transferred in utero, or via equipment or...
Toxic Plants to Horses
There are many poisonous plants in Wisconsin that could be a potential hazard to horses. These plants may cause symptoms such as: Colic Muscle weakness Incoordination Depression Paralysis Death Undesired plants can be eliminated in pastures by several methods,...
Senior Pet Care
There are many changes that can occur in our pets as they age. These changes may require us to care for them differently than we may have when they were younger. This guide is intended to help you recognize the signs or symptoms common in our senior pets and ways to...
Conservative Management of Arthritis
Weight Control Maintaining a healthy weight may be the most important element in assuring the best possible quality of life for a dog with osteoarthritis. Body weight not only increases the load on all joints, but inflammatory proteins produced by fat cells can cause...
Intestinal Parasites in Dogs and Cats
Parasites, or worms, are organisms that live at the expense of other animals. Dogs and cats commonly host parasitic infections which may be a health concern for both you and your pet. Intestinal parasites live primarily in the stomach and intestines where they feed...
Laparoscopic Ovariectomy: A Less Painful Alternative
Laparoscopic ovariectomy is a minimally invasive surgical technique used to remove the ovaries in female dogs. An ovariectomy differs from an ovariohysterectomy (spay) in that only the ovaries are removed, leaving the uterus in place. Both surgeries accomplish the...
Tick Transmitted Diseases
Lyme disease is contracted from the bite of a deer tick infected with a spirochete organism named Borrelia burgdorferi. The majority of dogs infected with the Lyme organism do not feel sick or have any clinical signs. Clinical signs include lameness, stiffness,...
Slow Feeders and Interactive Toys
Increased speed of eating can predispose our pets to: Excessive food intake resulting in obesity Poor digestion and vomiting Increased risk of swallowing air leading to bloating and abdominal discomfort Increased risk of GDV in dogs (gastric dilatation and volvulus:...