One Dose. Once a Year. LVC is proud to now offer ProHeart 12 to our patients as a new option for heartworm prevention! ProHeart 12 is the only once-yearly injection to prevent heartworm disease and intestinal parasites in dogs. Heartworm disease is on the rise in...
Dogs
Heartworm disease is on the rise in our area – keep your pets protected!
At Lodi Veterinary Care, we have seen at sharp increase in heartworm positive cases over the past year. We previously averaged 1-2 dog heartworm positive cases over this time, however, over the past six months, we have averaged 1-2 cases per month. This is scary!!...
Are grain-free diets harmful to your dog?
The FDA is currently researching a potential link between grain free dog food and development of heart disease. Grain-free food may lack taurine, an essential ingredient for your dog's heart health. Grain-free dog foods are high in carbohydrates, such as peas,...
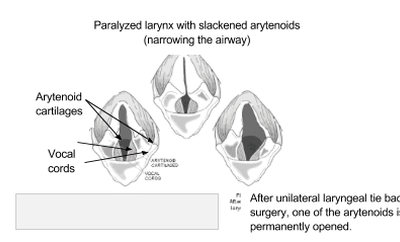
Laryngeal Paralysis
The larynx (or voice box) is a structure located in the throat that helps direct air into the lungs and food into the esophagus. Its function is important in preventing food/water from entering the lower airways when swallowing. The larynx opening and closing is...
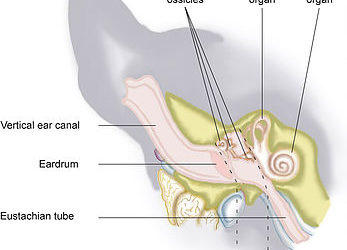
Vestibular Disease
The vestibular system is a combination of sensing receptors in the middle ear which help us determine our orientation and movement. These receptors then send signals via nerves to parts of the brain that help us maintain balance and coordinate our movements. If any...
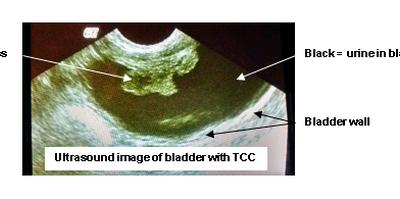
Transitional Cell Carcinoma (TCC)
Transitional Cell Carcinoma (TCC) is a cancer of the urinary bladder. Transitional cells are the cells that line the bladder wall, TCC is a cancer that arises from these cells. The exact cause is unknown, however, an increased risk of this cancer is found in certain...
Keratoconjucntivitis Sicca (KCS)
Keratoconjunctivitis sicca, otherwise known as KCS or Dry Eye is a condition in which tear production is abnormally low. Symptoms may include one or more of the following: Dry appearance to the eye Increased thick ocular discharge Conjunctivitis – red/inflamed eyes...
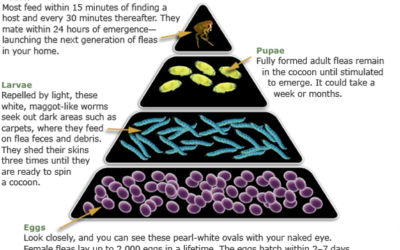
Flea Control Guide
How to Look for Fleas on Your Pet Examine your pet's coat carefully. Using a fine-toothed comb (flea comb), look for adult fleas, or for specks that look like pepper (flea dirt). The most common areas to find fleas/flea dirt are the groin, armpits, tailhead, and the...
How-To: Giving Subcutaneous (SQ) Vitamin B12 Injection
Take a new syringe from the package (syringes are single use only, call or visit us to get refills on syringes when needed) Draw up 0.25ml of the red Vitamin B12 solution (measure from the top of the black plunger). Pull up the skin between the shoulder blades to...
How-To: Cleaning Ears
Physical Exam and Ear Swabs – WHY? It is important to have an exam by the doctor and perform diagnostics (i.e. Ear Swabs) to determine the cause of the ear infection. The doctor must evaluate the ear drum to verify it is intact before prescribing ear medication, as...