One Dose. Once a Year. LVC is proud to now offer ProHeart 12 to our patients as a new option for heartworm prevention! ProHeart 12 is the only once-yearly injection to prevent heartworm disease and intestinal parasites in dogs. Heartworm disease is on the rise in...
Cats
Feline Diabetes Mellitus
Diabetes mellitus is a common problem in cats. Caring for a diabetic animal requires some effort, but most pets remain happy and comfortable. Successful patient management requires a team effort between you and our veterinary care team. What is diabetes mellitus?...
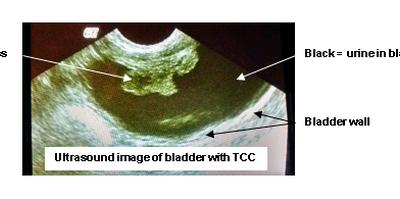
Transitional Cell Carcinoma (TCC)
Transitional Cell Carcinoma (TCC) is a cancer of the urinary bladder. Transitional cells are the cells that line the bladder wall, TCC is a cancer that arises from these cells. The exact cause is unknown, however, an increased risk of this cancer is found in certain...
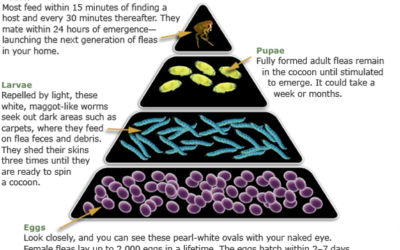
Flea Control Guide
How to Look for Fleas on Your Pet Examine your pet's coat carefully. Using a fine-toothed comb (flea comb), look for adult fleas, or for specks that look like pepper (flea dirt). The most common areas to find fleas/flea dirt are the groin, armpits, tailhead, and the...
How-To: Giving Subcutaneous (SQ) Vitamin B12 Injection
Take a new syringe from the package (syringes are single use only, call or visit us to get refills on syringes when needed) Draw up 0.25ml of the red Vitamin B12 solution (measure from the top of the black plunger). Pull up the skin between the shoulder blades to...
How-To: Giving a Pill to a Cat
One thing to keep in mind is that cats will do their best to make pilling difficult. Cats are not too fond of having their mouths pried open, let alone allowing you to insert a pill in their mouth. Some cats will salivate excessively, so it is very important that you...
How-To: Cleaning Ears
Physical Exam and Ear Swabs – WHY? It is important to have an exam by the doctor and perform diagnostics (i.e. Ear Swabs) to determine the cause of the ear infection. The doctor must evaluate the ear drum to verify it is intact before prescribing ear medication, as...
Senior Pet Care
There are many changes that can occur in our pets as they age. These changes may require us to care for them differently than we may have when they were younger. This guide is intended to help you recognize the signs or symptoms common in our senior pets and ways to...
Alternatives to Declawing
Scratching is a normal behavior of cats. Scratching allows cats to exercise, mark territory, condition the claws, stretch, and defend themselves. Many cats can be trained to scratch only on appropriate surfaces. In some cases, cats may excessively scratch or scratch...
Feline Litter Box Management Guidelines
There are many reasons why your cat may urinate/defecate inappropriately outside the litter box. Our friendly feline companions may eliminate inappropriately due to medical or behavioral reasons. If any inappropriate elimination, urination or defecation, is observed,...