by Lodi Vet | May 3, 2017 | Cats, Educational Materials
Feline Lower Urinary Tract Disease (FLUTD) describes the one or more from the following group of clinical signs:
- Bloody urine
- Straining and/or pain when urinating
- Urinating in unusual places
- Urinary blockage
- Over grooming the external genitals
These symptoms can occur as an isolated incident, however, many cats with FLUTD will have recurrent urinary problems throughout their lives.
The cause of this disease is variable, but can include:
- Stress, urinary tract infection
- Crystals in the urine
- Bladder stones
- Urinary tract cancer or polyps
- Trauma to the urinary tract
Diagnostic testing is important in helping sort out the cause of the urinary symptoms. These tests often include:
- Blood testing (to rule out kidney disease)
- Urinalysis
- Urine culture (to determine the type of bacteria present and which antibiotic will work best to treat it)
- Ultrasound and/or x-ray of the urinary tract
In 50% of the cases, a cause cannot be determined despite extensive testing, this clinical syndrome is called “idiopathic cystitis.”
Treatment is based on the cause. In cases of “idiopathic cystitis” many modalities may be used through trial-and-error to control symptoms but a cure can be difficult to achieve.
Common treatments for specific ailments include:
- Urinary infections are treated with antibiotics
- Crystals in the urine are treated with diet change
- Painful urination is treated with anti-inflammatory of pain relieving medications
- Bladder stones are treated with surgical removal
- Stress can be managed with pheromones, diet change, behavior modification and medications.
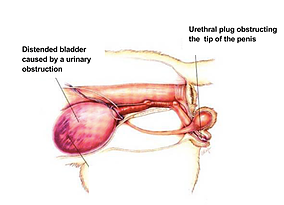 Urinary Obstruction/Blockage
Urinary Obstruction/Blockage
Male cats experiencing lower urinary tract disease are uniquely at risk for a life threatening complication of this syndrome – urinary obstruction. Blood, crystals, stones and mucus can form a plug that clogs the narrow male urethra preventing urine from passing. If this blockage persists, it can lead to bladder rupture or changes in the blood that can result in severe illness or death.
Initial treatment involves placing a urinary catheter under sedation/anesthesia to allow the bladder to empty. The urinary catheter may be left within the urethra for continued urine passage for 24-48 hours allowing for treatment of the inciting cause.
Cats that have had a urinary obstruction will be at significantly higher risk of re-blocking in the future. Some male cats with frequent incidence of urinary blockage will be advised to undergo a surgical reconstruction of the genitalia to create a more female-like opening to allow for easier passage of urine. This surgery is called a perineal urethrostomy (or “PU” for short). If this procedure is needed, your veterinarian will discuss the details of this procedure with you.
by Lodi Vet | May 3, 2017 | Dogs, Educational Materials
Canine cutaneous histiocytomas are common tumors that are unique to the dog. They occur most often in young dogs, but can be seen in dogs of any age. Histiocytomas can be found in any breed, but are most common in Labradors, Staffordshire terriers, Dachshunds and Boxers.
Histiocytomas can often be diagnosed by fine needle aspiration. The cells that comprise a histiocytoma have a characteristic microscopic appearance. Histiocytomas usually occur as a solitary, fast growing, non-painful, dome shaped lesion in the skin. Usually the surface is shiny and hairless, but with time they can become raw and ulcerated.
Although histiocytomas are classified as tumors, they are unique in that they are benign and often regress and disappear without treatment. Those that do not regress on their owner should be surgically removed and submitted for histopathology to confirm that they are indeed histiocytomas. There is another type of mass that is similar appearance to histiocytoma that can be more aggressive or malignant, therefore removal of any masses that are not resolving on their own is important. The prognosis for surgical removal of the histiocytoma is excellent.
The recommended treatment course is typically time and close monitoring. Surgery may be advised based on history, location, appearance and results of fine needle aspiration. It is important to maintain good communication until the growth completely regresses or is surgically removed.
by Lodi Vet | May 3, 2017 | Cats, Educational Materials, How To
Most cats are very uncomfortable with a container being slipped underneath them when they are in their litter box, so it is a bit of a challenge to obtain a clean urine sample from a cat. To aid you in this adventure, we have put together some suggestions to help make the process easier for you. Because all cats are different in their litter box preference, you may need to try more than one of the following suggestions or a combination of a couple of them to find your cat’s preference. Please feel free to contact us at any point with questions.
- First, completely clean out the litter box (washing thoroughly with soap & water to remove any dust), then place the No-Sorb beads in place of your regular litter. No-sorb beads prevent urine from being absorbed. After the cat urinates, the beads and urine can be put back into the collection container and brought to the hospital.
- Cats are sometime texture driven, therefore, other substances can be used in place of the No-Sorb beads. Other safe materials include; dust free dried beans, polystyrene packing peanuts (non-dissolvable), or clean aquarium gravel.
- Another method is to place a piece of plastic sheeting over the existing litter. This can be done with a couple of layers of saran wrap or by placing the entire litter box in a plastic garbage bag. Make sure the plastic lays flat against the litter. The cat will feel the litter under their feet and use the box as they normally would. You can then retrieve the urine sample with the syringe provided.
If your cat is uncooperative in any of the above methods, we can help by setting up an appointment for a cystocentisis. Cystocentisis is done by passing a needle into the bladder and obtaining a sample directly. Although this sounds unpleasant, it is surprising how well cats tolerate the procedure. It is important to keep your cat away from their litter box for at least two hours prior to this appointment.
After obtaining the sample, it is extremely important to get the sample to us in a reasonable amount of time. For best results, the sample should be processed within 2 hours after collection. If that is not possible, the sample should be refrigerated and tested within 6 hours.
by Lodi Vet | May 3, 2017 | Cats, Educational Materials
The thyroid glands are located in the neck and play a vital role in regulating thebody’s metabolic rate. Hyperthyroidism is a disorder characterized by the overproduction of thyroid hormone and a subsequent increase in metabolic rate. The thyroid gland enlarges with hyperthyroidism, however this is generally a benign or non-malignant change. Less than 2% of hyperthyroid cases involve malignant thyroid gland tumors.
What causes hyperthyroidism?
Older cats are at increased risk for developing hyperthyroidism. Environmental and dietary risk factors have been investigated but there has been no correlation identified. No individual breed is known to be at increased risk, although the Siamese appears to have a somewhat increased incidence of hyperthyroidism compared to other breeds.
What are the clinical signs of hyperthyroidism?
Cats with hyperthyroidism are usually middle-aged or older. The average age of affected cats is approximately twelve years. The most common clinical sign of hyperthyroidism is weight loss secondary to the increased rate of metabolism. The cat tries to compensate for this with an increased appetite. Despite the increased food intake, most cats continue to lose weight. Affected cats often have increased water consumption and urination, as well as intermittent vomiting or diarrhea. Their fur may appear unkempt due to decreased grooming.
There are two secondary complications of hyperthyroidism that can be significant. These include hypertension (high blood pressure) and heart disease called thyrotoxic cardiomyopathy.
Heart problems develop because the heart must enlarge and thicken to meet the increased metabolic demands. In some cases, the cat will develop a heart murmur associated with the cardiomyopathy. Hypertension develops due to the increased pumping pressure and elevated heart rate that occurs with thyrotoxic cardiomyopathy.
Both cardiomyopathy and hypertension are potentially reversible with appropriate treatment of hyperthyroidism.
Hyperthyroidism also plays a role in kidney function. Uncontrolled hyperthyroidism increases the blood flow to the kidneys, which can mask underlying kidney disease. Kidney function needs to be closely monitored, especially during initial treatment of hyperthyroidism, to find appropriate balance between management of hyperthyroidism and kidney function.
How is hyperthyroidism diagnosed?
In most instances, diagnosis of this disease is relatively straightforward. The first step is to determine the level of one of the thyroid hormones, called total thyroxine (TT4). Generally, the TT4 level is so high that there is no question as to the diagnosis. Occasionally, a cat that is suspected of having hyperthyroidism has a TT4 level within the upper range of normal. When this occurs, a second test, usually a free T4, is performed.
What is the prognosis for hyperthyroidism?
The outcome of treatment for hyperthyroidism is usually excellent and most cats have a very good chance of returning to a normal state of health.
How is hyperthyroidism treated?
Treatment of hyperthyroidism is usually very successful. Tests are needed to evaluate the overall health and help predict the chances for any treatment complications. Such tests include bloodwork, urinalysis, and blood pressure – often these have already been performed as part of original testing. Additional diagnostics may include chest radiographs and ECG to further evaluate the heart.
Methimazole oral or transdermal medication.
- Methimazole blocks the production of excess thyroid hormone and is a life-long medication.
- It is available in an oral tablet called Felimazole at our hospital. It can also be prescribed in liquid form at specific pharmacies.
- For cats that are a challenge to administer oral medication, methimazole can be compounded into a transdermal gel that is applied to the skin on the inner aspect of the ear for absorption.
- Regular blood screening and blood pressure monitoring are needed to assess disease control.
- Potential side effects of oral methimazole include vomiting and/or diarrhea, facial scratching/excoriation, and in very rare instances bone marrow suppression. If present, other treatment options should be pursued.
Radioactive iodine. A very effective way to treat hyperthyroidism is with radioactive iodine (I 131).
- An injection of radioactive iodine is given intravenously and it destroys the abnormal thyroid tissue without endangering other organs.
- 95% of cats require no further treatment for hyperthyroidism after radioactive iodine treatment.
- Treatment requires 2-3 days of hospitalization at a veterinary hospital licensed to administer radiation therapy – the closest in our area is UW Veterinary Care in Madison. Approximate cost is $1500.
- There is more upfront cost with this treatment, but often is most cost effective in long-term due to no need for continued medication.
Hill’s y/d diet.
- For cats that do not tolerate methimazole or other treatment options, Hill’s y/d diet is an alternative treatment option.
- Hill’s y/d very tightly limits iodine intake to control thyroid hormone (T4) production. When fed, it is the sole treatment used – the diet is not used in combination with methimazole or radioactive iodine.
- Routine blood screening and blood pressure monitoring is needed for proper disease management.
- It is not ideal for multi-cat households or indoor/outdoor cats.
We will work together to find the best treatment for your cat’s hyperthyroidism. Please contact us with any questions or concerns regarding this information.
by Lodi Vet | May 3, 2017 | Dogs, Educational Materials
Addison’s disease is a condition affecting the adrenal glands. The adrenal glands are located near each of your pet’s kidneys. These glands are responsible for releasing hormones that maintain water balance and regulate electrolytes; sodium, potassium and chloride. Addison’s disease causes the adrenal glands to release less than normal amounts of these hormones. During times of stress, these hormones are needed by your pet’s body.
When the adrenal glands do not function normally, your pet can become severely dehydrated, become lethargic or tired, develop low blood sugar, and begin vomiting and/or have episodes of diarrhea. Animals can go into shock and die from this condition if left untreated.
Diagnosis
To diagnose Addison’s disease, we perform blood tests that help us narrow down the problem by checking electrolytes and kidney values. Doctors must also rule out other causes for symptoms. If the doctor interprets abnormalities in the initial bloodwork that indicates a concern of Addison’s disease, they will request an ACTH stimulation test to be done. This test will confirm the final diagnosis of Addison’s Disease. The ACTH test challenges the adrenal glands. If your pet has Addison’s disease, the adrenal glands will not release enough hormone to properly respond to the stimulus.
Treatment
Treatment consists of fluid therapy to improve hydration and medications to replace the hormones that the adrenal glands are not releasing properly. Long term management includes an oral corticosteroid supplementation and a monthly injection of DOCP. DOCP is a medication that helps the body manage electrolytes. DOCP should be administered by our team of doctors and technicians until your pet is fully regulated. Once regulated you may choose to administer the DOCP at home. There are other medications available, but this is the most common treatment.
Once diagnosed, Addison’s Disease is a life-long condition, and will require treatment and monitoring. However, with treatment and monitoring, most animals with Addison’s disease can live a long and happy life.
by Lodi Vet | May 3, 2017 | Dogs, Educational Materials
Kennel cough is a common contagious illness that develops in dogs that have been mingling with other infected animals. This can occur through boarding, grooming, dog parks, pet stores, family gatherings or nose-to-nose contact while out on walks through the neighborhood.
Causes of kennel cough can include both viruses and bacteria. Commonly, more than one agent is involved in an infection. Infections with the following organisms have been implicated in creating kennel cough:
- Bordetella bronchiseptica (bacteria)
- Parainfluenza virus
- Adenovirus type 2
- Canine distemper virus
- Canine influenza virus
- Canine herpes virus
- Mycoplasma canis (a single cell organism that is neither virus nor bacteria)
The main symptom of kennel cough is a hacking cough. Pet owners will often describe this cough as sounding like “something is stuck in the throat.” Occasionally fever, sneezing, nasal or ocular discharge can also be seen. The incubation period (the time from exposure to clinical signs) is 2-14 days. Dogs are typically sick for 1-2 weeks and infected dogs can shed kennel cough organisms for 2-3 months after infection. In complicated cases, or in pets with compromised airways, pneumonia may result.
The diagnosis of kennel cough is typically made based on history of exposure to other dogs within the proper timeframe, plus typical exam findings of a coughing dog that is otherwise feeling well is adequate to make the diagnosis. (Source: VeterinaryPartner.com). Radiographs can be helpful to show signs of bronchitis or pneumonia in complicated cases.
Treatment involves antibiotics and occasionally cough suppressants. Warm humid air therapy (by using humidifiers or allowing pets to sit in a bathroom while a warm shower is running) can also be used in helping a pet clear their airways.
Vaccines are available to help protect against kennel cough, however the vaccines are not expected to completely eliminate the risk of infection. Vaccinated dogs generally have milder symptoms than unvaccinated dogs. Any dogs with lifestyles that predispose them to infection (grooming, boarding, training groups, dog parks, daycare, etc.) are strongly advised to receive regular vaccinations to help reduce their risk.
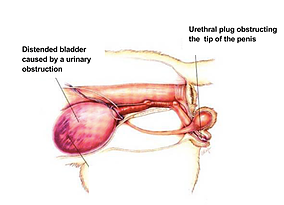 Urinary Obstruction/Blockage
Urinary Obstruction/Blockage