by Lodi Vet | Jun 15, 2017 | Dogs, Educational Materials
Grapes and raisins can be toxic to dogs resulting in kidney failure. It is unknown at this time which part of the grape causes toxicity. Ingestion of as little as 1 or 2 grapes can result in toxicity. Not every dog or cat is susceptible and some dogs can tolerate large quantities of grapes or raisins without any clinical signs. Unfortunately, it cannot be determined which pets will experience toxicity and which will not. Currently, there is no information about whether or not grape juice might be toxic.
Clinical signs can be seen within a few hours. These include: vomiting, lethargy and decreased appetite. Other signs of kidney failure such as reduced or lack of urine production can happen within 24 hours.
For immediate ingestion, induction of vomiting is indicated. If vomiting is unsuccessful or if ingestion was too long ago for vomiting to be helpful then charcoal administration and aggressive intravenous fluid therapy will be necessary. Unfortunately, even with early and aggressive treatment prognosis is poor if signs of kidney failure appear as a result of raisin/grape toxicity.
If you think you pet may have eaten raisins or grapes please call us at 608-592-3232 immediately.
by Lodi Vet | Jun 15, 2017 | Dogs, Educational Materials
Hot spots are a common dermatologic condition of dogs. Hot spots are the result of a superficial skin infection – in the early stages the skin will turn red, become moist and itchy. Often hair loss will occur as a result of chewing and infection. Frequently this area will be painful to the touch. As time progresses a dried scab or crust will form.
The exact cause of a hot spot can be anything that results in itch or irritation to the skin causing a dog to chew or lick at an area. Possible causes can include: allergies, insect bites, scrapes, clipper burn from grooming, injuries, matted fur, or moisture accumulation in skin folds.
Diagnosis is often made by physical exam and cytology (microscopic evaluation of the discharge on the skin). The cytology helps determine if the area is infected with bacteria, yeast or both. If bacteria are detected, culture and sensitivity testing may be used to choose the most appropriate antibiotic to treat the infection.
Treatment may involve one or more of the following:
- Clipping the hair away from the affected area
- Cleansing the skin with antibacterial shampoos
- Topical anti-inflammatories or antibiotics
- Oral antibiotics or antifungals
- Oral medications to reduce inflammation or itch
- Prevention of licking with E-collar or medical pet shirt
by Lodi Vet | Jun 5, 2017 | Educational Materials, Equine
Would you recognize choke in your horse?
The word choke is a bit of a misnomer in the horse. In people it refers to an obstruction of the trachea or windpipe, usually with a piece of food. In horses the obstruction is of the esophagus not of the airway. This means that usually choke in horses is not immediately life threatening, however long term complications can result if the choke does not resolve on its own or is not treated in a timely fashion.
What causes choke?
Choke can be caused by many different types of feed. Most commonly grain or hay, but beet pulp, corn cobs, apples and carrots have been implicated as well. Horses choke on feed either because the feed is too large to pass down the esophagus, such as with a large apple or carrot, or because the feed expanded after being wet with saliva and swallowed in too large an amount, such as with beet pulp or grain. If choke is caused by hay it is likely due to a large portion of the hay being swallowed without sufficient breakdown, or chewing, prior to swallowing.
What does choke look like in the horse?
The most common sign of choke is a large amount of saliva or feed discharge from both nostrils due to the horse’s inability to swallow. The horse may repeatedly extend their neck, cough, and gag and make attempts to swallow. Sometimes if the obstruction is large enough and is located in the upper esophagus it can be seen and/or palpated on examination.
What predisposes horses to choke?
The most common reason for choke in horses is poor dentition. If there are missing teeth or dental issues such as a wave mouth or teeth that are too worn to chew properly this can result in improper feed breakdown prior to swallowing. That being said we occasionally run across horses that have normal teeth that just eat too fast for their own good! Regardless of the inciting cause of the choke often we have to modify the diet or modify the feeding process in some way to try and help prevent re-occurrence.
How do I treat it?
If you notice these signs in your horse it is very important to call your veterinarian. The sooner the choke is treated the less of a chance there is of complications. Treatment includes sedation to help relax the horse and the esophagus and passing a tube to help pass or flush out the obstruction. Other treatments can include pain medication, anti-inflammatory medication, antibiotics and oftentimes oral rehydration as the horse was unable to eat or drink while choked. Your veterinarian will likely determine which treatments are required depending on the type of choke and the length of time the horse has been choked.
by Lodi Vet | Jun 5, 2017 | Educational Materials, Equine
Laminitis is the inflammation of the tissues which connect the hoof wall to the coffin bone. This can occur in horses of any age, sex and size, and it can occur due to multiple factors. Severity may range from mild to very severe cases in which euthanasia may be recommended as the most humane option. Some cases are of short duration and others may lead to chronic conditions that cause permanent lameness. Each year approximately 1.4% of the horse and pony population suffers from acute laminitis, and another 1.8% struggles with chronic laminitis.
Some risk factors for laminitis include:
- over consumption of lush pasture
- excessive grain
- obesity
- equine metabolic syndrome or equine cushings
- mares who retain their placenta after foaling
- weight bearing injuries placing extra stress on opposite limbs
- trauma or injury to a limb or hoof
- exposure to toxic substances, i.e. black walnut shavings
- diarrhea or other systemic infections
- long term or excessive steroid use
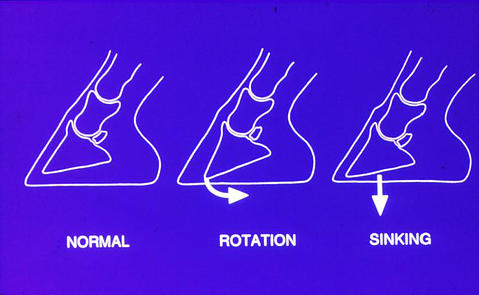
“Founder” describes a subset of laminitis cases in which the coffin bone rotates away from the hoof capsule.
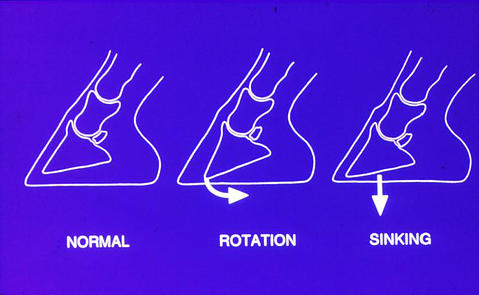
So what signs do we look for when determining if a horse or pony has laminitis? Clinical signs include a reluctance to move and lameness especially in the front limbs, lethargy, sweating, and increased respiratory and heart rate. Affected horses may be resistant to pick up their feet, have a difficult time turning, have a characteristic “saw horse” stance, and are more painful on hard ground. Some horses may spend an increased amount of time lying down. In more mild cases, the horse may simply appear stiff.

Characteristic laminitis stance with the front limbs extended in front, and the hind limbs positioned under the body to bare more of the horse’s weight.
Your veterinarian will do an exam of your horse, as well as discuss a complete history of your horse to determine if he or she is affected by laminitis. An exam may include hoof testing, nerve blocks, and x-rays. Bloodwork or other diagnostics may also be recommended depending on the case.
Prevention is key! Limit grazing and/or use a grazing muzzle prevent weight gain or assist with weight loss in obese horses. Proper hoof care every 6-8 weeks, with shoeing if needed, is important. If the horses are not laminitic, exercise can aid in facilitating weight loss. Watch for clinical signs of Metabolic Syndrome (young to middle aged horses, excess fat deposition, weight gain, lameness) or Cushing’s (horses 15 years and older, excessive weight gain, long hair coat, excess sweating, increased drinking and urination, recurrent infections or lameness) and schedule an appointment with your veterinarian if any of those signs are noted.
Treatment for laminitis may include:
- Anti-inflammatory medications (ex. bute, DMSO)
- Stall rest or exercise restriction
- Deep bedding or sand, or special boots to provide cushion for the feet
- Dietary restriction: grass hay and a vitamin/mineral supplement. No grass or grain!
- Proper medical treatment for other health concerns (ex. treatment of Cushing’s if present)
- Mechanical support with trimming +/- shoes
- Ice or cold-water therapy to the distal limbs where feasible
- Other therapies may be recommended on a case-by-case basis
If you see signs of laminitis in your horse or risk factors for developing laminitis, do not hesitate to call your veterinarian. Laminitis is considered an emergency as it can cause serious life-altering changes if left untreated. Remember, it is always better to prevent this disease rather than treating it.
by Lodi Vet | Jun 5, 2017 | Educational Materials, Equine
Overheating can be a serious problem in horses. More often this is an issue in summer with warm, humid weather; yet it can occur at all times of the year. As in any species, overweight horses are more prone to overheating. Any sort of breeze, even those supplied artificially with fans can help to cool your equine friends due to convection cooling with sweating and the subsequent heat loss during drying.
To determine if your horse is at risk for overheating monitor your horses’ basic health parameters such as rate of breathing, rectal temperature, capillary refill time and attitude.
- Start with their breathing by observing their abdomen rise and fall. Increased respiratory rate is normal after exercise and should decrease within a few minutes of activity stopping. If your horse continues to breathe heavily, this may be of concern.
- Taking a temperature rectally with a thermometer is also useful. A thermometer from your local pharmacy is adequate. Temperatures elevated above 102.5 F after cool down or at rest if out on pasture, justifies a call to your veterinarian.
- Overall attitude can relay how a horse is feeling. An overheating horse may be uninterested in their surroundings, hanging their head, or not willing to eat grass or feed that’s offered.
- Capillary refill time is checked by pressing a finger against the gums or gingiva above the front incisor teeth to cause the color to fade and return. Normal color should be light pink to pink. After the gingiva is pressed color should return in less than 2-3 seconds. Also take note of how much moisture is present when touching your horse’s gums, as tacky or dry gingiva can relate to dehydration.
To cool an overheating horse, start with hosing them off with cool water. Avoid using ice cold water as this may be a shock to your equine companion. After a cool bath, be sure to remove the excess water from his or her coat using your hand or a sweat scraper. This water can trap heat and act in an insulating fashion, rather than continuing to cool their temperature. Place your horse in a shaded area with a cool breeze or fan to continue the cooling process. Always offer free choice, fresh, cool water for drinking. After exercise small drinks of water are preferred during cool down.
Sweating is the natural way for horses to cool body temperature down. Along with loss of water, horses loose important electrolytes in their sweat. These electrolytes are minerals such as potassium, chloride, sodium and smaller amounts of calcium, and magnesium. Working horses or those that are sweating in hot weather can benefit from electrolyte supplementation even if they have a mineral block available. Options for supplementation include regular salt (sodium chloride) or light salt (potassium chloride) added to grain, water, or offered free choice. No more than 2 tablespoons per day should be added to grain for a full sized horse. If electrolyte water is offered, regular water should be available at all times as well. Horses that are used to salt blocks and licks should be gradually transitioned to loose salt over 1-2 weeks to prevent over consumption. Another option is top dressed electrolyte mixes (Doctor’s Choice-Recharge is offered at Lodi Veterinary Care) or oral pastes such as Electro-plex can be given.
If your horse does not show signs of sweating during conditions where they would normally be expected to, he/she may have a more severe condition occurring called anhidrosis. We urge you and your pets to stay cool during this summer’s heat wave. Please do not hesitate to call should questions arise.
by Lodi Vet | May 3, 2017 | Cats, Educational Materials
Feline upper respiratory infections are a common cause of nasal congestion, sneezing and ocular discharge in cats. Occasionally these cats will have more severe symptoms like a fever, cough, and decreased appetite as the infection progresses.
Causes of feline respiratory infections are primarily viruses. The most common viruses implicated are herpesvirus and calicivirus. Secondary bacterial invaders will take advantage of the weakened immune system resulting in worsening of the symptoms. Cats contract these viruses and bacteria by other infected cats. Most commonly this occurs in cats recently adopted from shelters or rescue groups, after boarding, or in cats that spend time outdoors or those that have contact with cats who spend time outdoors. These viruses are highly contagious and once infected, a cat can shed the virus intermittently throughout their lives. Stress can cause recrudescence (flare up) of a previously contracted respiratory virus.
Diagnosis is made by physical exam and history. In complicated cases radiographs, blood panels or viral testing may be warranted.
Treatment is often based on the severity of clinical signs but may include one or more of the following:
- Warm humid air therapy (spending time in bathroom when a hot shower is running, or having a warm air humidifier nearby) This can help reduce nasal congestion
- Antibiotics if there is indication of a secondary bacterial infection
- Medicated eye drops/ointment
- Fluids may be given under the skin if dehydration is suspected
- Warming canned food can help encourage a better appetite
Infected cats should be kept indoors to monitor clinical signs and response to treatment.
Most feline respiratory infections run their course in 10-14 days, however cats can remain infectious for months. It is important to keep in mind that once infected cats may have