by Lodi Vet | Apr 12, 2017 | Dogs, Educational Materials, Home Page, Wellness
Laparoscopic ovariectomy is a minimally invasive surgical technique used to remove the ovaries in female dogs. An ovariectomy differs from an ovariohysterectomy (spay) in that only the ovaries are removed, leaving the uterus in place. Both surgeries accomplish the same goal of making a dog unable to conceive and eliminating heat cycles. It is safe to only remove the ovaries, as risk of pyometra (severe uterine infection) is 100% eliminated with complete removal of ovaries.
Advantages of Laparoscopic Ovariectomy
- Smaller (~1cm) incisions, less painful
- Shorter recovery time
- Controlled cautery of blood vessels minimizes pain and bruising
- Magnification allows for optimal visualization of abdominal organs
 A traditional spay is an open abdominal surgery through one large incision. A ligament, called the ovarian suspensory ligament, is torn to release the ovary so that it can be removed from the abdomen and the blood vessels are “tied off” (ligated). This ligament tearing causes the majority of post-operative pain and leads to bruising within the abdomen.
A traditional spay is an open abdominal surgery through one large incision. A ligament, called the ovarian suspensory ligament, is torn to release the ovary so that it can be removed from the abdomen and the blood vessels are “tied off” (ligated). This ligament tearing causes the majority of post-operative pain and leads to bruising within the abdomen.
A laparoscopic ovariectomy is performed using a small, thin camera and surgical instruments inserted into the abdomen through two small port incisions. The ovarian suspensory ligament is carefully cauterized and cut under direct visualization, rather than torn by feel. We utilize a Miseal®, an advanced surgical device, to thermally fuse the ligament and blood vessels.
Please contact us with any questions regarding these procedures – we can provide additional information and help determine if a laparoscopic ovariectomy is best for your dog.
by Lodi Vet | Apr 12, 2017 | Cats, Dogs, Educational Materials
As pet owners, we want to provide the best medical care we can for our pets and minimize the discomfort of testing. Our pets can’t tell us when they are in pain so often they need more diagnostics when they are “not right”.
Endoscopic procedures provide a safe, less painful way to provide an early diagnosis of many disorders in a minimally invasive way and allow specific therapeutic treatments.

Endoscopic Retrieval of Foreign Material
Flexible Endoscopy
This type of endoscopy involves using a flexible tube with a viewing port and a video camera that can be inserted into the esophagus and stomach through the mouth or into the colon via the rectum. This allows our doctors to image and biopsy the esophagus, stomach and colon without surgery. Foreign bodies can often be retrieved from the stomach and esophagus using endoscopy, saving pets from having to go through open abdominal surgery.
Rigid endoscopy
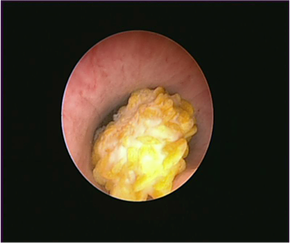
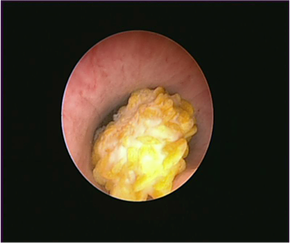
Cystoscopy showing large stone within bladder
This type of endoscopy involves using a shorter, more rigid endoscope to evaluate areas such as the nasal passages and urinary bladder. Rhinoscopy is performed to look, flush and biopsy inside the nasal passage to help determine causes of sneezing, reverse sneezing, nasal discharge and abnormally loud breathing sounds. Cystoscopy is performed to look within bladder and allow biopsy of bladder tissue to help determine the cause of blood in urine and/or abnormal urination.
Our goal at Lodi Veterinary Care is to provide leading edge diagnostics and quality medicine for your pets. Please contact our office if you have any questions about these diagnostics or to discuss if you think your pet would benefit from any of these procedures.
by Lodi Vet | Mar 31, 2017 | Cats, Dogs, Educational Materials, Wellness
Lyme disease is contracted from the bite of a deer tick infected with a spirochete organism named Borrelia burgdorferi. The majority of dogs infected with the Lyme organism do not feel sick or have any clinical signs. Clinical signs include lameness, stiffness, swelling of limbs or joints, fever, lethargy, reluctance to move, loss of appetite, vomiting or depression. On occasion, Lyme disease presents with kidney damage which occurs when the immune system is exposed to the Lyme spirochete over a period of time.
A simple blood test can determine if your dog has been exposed to the Lyme organism. A positive test (or titer) simply means your dog has been exposed. If the test is positive, further blood and urine tests are recommended to determine how the dog is responding to the organism.
After Lyme disease is diagnosed (based on further blood and urine test or clinical signs) the treatment is a four week course of antibiotics. The clinical signs typically improve rapidly within 48 hours. Treatment does not always eliminate the organism from the body which is why titers often remain positive even after treatment.
The best way to prevent Lyme disease is through strict adherence to tick control and vaccination protocol. Statistically, the majority of the dogs in our area are at risk for encountering the ticks that carry Lyme disease and the vaccination is strongly recommended for most dogs in our area. It is best to vaccinate early in life before exposure. A Lyme test may be advised prior to vaccinating to know if there has already been exposure. After the initial series, the Lyme vaccination is boostered yearly.
At Lodi Veterinary Care, we recommend these tick/flea products: Simparica (oral monthly tablet), or Parastar Plus (monthly topical). We also an additional oral option for puppies called Credelio. Ticks lay dormant over the winter but become active any day the temperature is above freezing. Year round application may be the safest option with the unpredictable winter temperatures.
Summary: Lyme disease is a very complicated disease.
- Many dogs are infected with the Lyme organism yet few develop the disease.
- Positive Lyme test does not equal disease
- The tests used in detecting Lyme disease have improved which has increased the value of testing
- Treatment is generally well tolerated and effective.
- Vaccinating young dogs before infection is strongly advised.
- Tick control is crucial to preventing all tick borne diseases. We advise Parastar Plus or Bravecto.
ANAPLASMOSIS (Anaplasma phagocytophilum)
Anaplasmosis is a disease caused by an organism similar to the Lyme spirochete and is transmitted by the deer tick. It can occur on its own, or as a co-infection with Lyme disease. Once in the body, the organism may or may not cause external signs of disease. It is impossible to predict which pets will be clinically normal (unapparent carriers) and which will actually get sick. The clinical signs include swollen joints, fever, lethargy, vomiting and diarrhea. As the disease progresses, there may be significant changes in the blood including low platelets and changes in the white blood cell counts. Occasionally, in early stages of the disease the organism can be found in the white blood cells.
There currently is not a vaccination available for Anaplasmosis. There is, however, a test to see if your dog has been exposed to the organism (Snap 4DX test). A positive test does not mean the pet is going to get sick from the disease, but does indicate exposure to the organism. Like Lyme disease, many dogs may test positive and be asymptomatic (show no clinical signs).
The protocol for Anaplasmosis starts with a blood screen to determine if and how the disease is affecting the body. If treatment is needed based on clinical signs or blood screen findings, a four week course of an antibiotic will be prescribed. Many pets will remain asymptomatic carriers and continue to test positive despite treatment. These dogs should continue to be carefully screened with the recommended blood work to monitor for any signs of the disease.
EHRLICHIOSIS (Ehrlichia canis)
Ehrlichiosis is another tick borne disease. It is caused by organisms similar to those that cause Lyme disease and Anaplasmosis. The clinical signs include lethargy, fever and swollen joints. Blood work may show low platelets, high protein levels, anemia, and elevated liver values. This disease can be a very chronic, slowly progressive disease. It is diagnosed with a positive Snap 4DX test followed by a medical workup. Treatment is a four week course of antibiotics if needed based on blood counts or clinical signs. There is not a vaccination available at this time. Like all tick borne diseases, your pet may test positive and not show any clinical signs (asymptomatic carrier). Infected dogs should continue to be carefully screened with the recommended blood work to monitor for any signs of the disease.
by Lodi Vet | Mar 31, 2017 | Educational Materials, Equine
It is the time of year when the clinic starts to see an increase in the number of tendon and ligament injuries due to horses fresh from the winter. The show season is getting heavy for many clients and their horse is unable to compete due to a tendon/ligament injury.
What can be done to treat the tendon or ligament injury?
One of the newest recommended treatments is Shockwave Therapy. This technology is based from a treatment used in humans that breaks up kidney stones. These high intensity ultrasound waves travel through fluid and soft tissue. When the injured tendon or ligament is hit with these waves, the tissue releases multiple healing factors to speed up the healing process. With this treatment the injury will heal twice as fast, compared to just rest. So, if a tendon is injured, the normal treatment is six to nine months of rest; shockwave treatment could potentially get your horse back to work in three months.
What else should be done?
With all tendon or ligament injuries, it is good to follow the healing process with an ultrasound. Before work is started, an ultrasound should be done to make sure the area is completely healed. This will prevent re-injury to the same areaa.
Where can I find a shockwave unit?
The clinic has their own shockwave unit. We are seeing good success at treating tendon injuries with shockwave therapy. The success rate is higher if the shockwave treatment is started shortly after the injury has occurred. Shockwave treatment does give some immediate pain relief.
Can I work my horse during this?
During this time the horse’s activity is highly restricted. A typical treatment plan using shockwave therapy is to start with aninitial treatment, then in two weeks have a follow up treatment. During this time the horse should be on stall rest with hand walking. It may be necessary to have one more treatment two weeks after the second treatment. This treatment plan varies with every case. It is also important not to let the horse have too much exercise within seven days after the treatments are done. A good rehabilitation schedule should be followed to obtain the best quality of healing. Shockwave therapy can also be used for a sore back, splints, joints, and non-healing wounds.
by Lodi Vet | Mar 10, 2017 | Dogs, Educational Materials
Hip dysplasia is a genetic malformation of the hip joint that is found most often in large breed dogs. The hip is a ball and socket joint. Hip dysplasia can be caused either by having a very shallow acetabulum (socket) or having a flattened or shortened femoral head (or ball portion of the ball and socket joint, which is attached to the thigh bone). Because of the incongruity of the ball and socket in these situations, this condition results in abnormal motion of the hip joint causing excessive “wear and tear” on the joint.
Symptoms of hip dysplasia can vary from no symptoms to more significant signs. The visible signs of hip dysplasia can include: lameness of the hind leg, abnormal swaying of the hips, discomfort upon rising and reluctance to run or jump. Long term these signs can progress to near crippling pain and decreased mobility from severe arthritis. Unfortunately, there is no way to predict how it will develop in each individual.
Diagnosis is made by a combination of physical exam signs and x-rays. The problem may not always be detectable by x-ray until 2 years of age. To avoid perpetuation of hip dysplasia, affected dogs should not be used for breeding. We recommend all potential breeding dogs be OFA (Orthopedic Foundation for Animals) certified as “dysplasia free” when they reach 2 years of age.
Treatment is designed to ease the symptoms and give your pet a more comfortable life, however there is no cure for hip dysplasia. Treatment may consist of the following:
- Medication – for stiffness and pain
- Artificial hip replacement surgery
- Surgical removal of the femoral head
- Weight reduction
by Lodi Vet | Mar 10, 2017 | Cats, Dogs, Educational Materials, Wellness
Increased speed of eating can predispose our pets to:
- Excessive food intake resulting in obesity
- Poor digestion and vomiting
- Increased risk of swallowing air leading to bloating and abdominal discomfort
- Increased risk of GDV in dogs (gastric dilatation and volvulus: bloating and twisting of the stomach – a surgical emergency)
Reducing the speed in which our pets eat can help improve their digestion and help reduce the risk of some of the negative side effects associated with fast eating. Various methods are available, not all methods are appropriate for every pet. Based on your pets personality and eating style one or more of these options may be helpful in slowing down their eating speed. Your veterinarian will be able to help you choose the right solution for your pet.
- Spread food over a cookie tray or the ground
- Put a coffee cup in the middle of your pet’s bowl
- Purchase a slow feeder or maze bowl
- Use a puzzle toy to slow feeding
 A traditional spay is an open abdominal surgery through one large incision. A ligament, called the ovarian suspensory ligament, is torn to release the ovary so that it can be removed from the abdomen and the blood vessels are “tied off” (ligated). This ligament tearing causes the majority of post-operative pain and leads to bruising within the abdomen.
A traditional spay is an open abdominal surgery through one large incision. A ligament, called the ovarian suspensory ligament, is torn to release the ovary so that it can be removed from the abdomen and the blood vessels are “tied off” (ligated). This ligament tearing causes the majority of post-operative pain and leads to bruising within the abdomen.