by Lodi Vet | Mar 10, 2017 | Cats, Dogs, Educational Materials
Giardia is a protozoa parasite that can affect both pets and humans resulting in diarrhea. It is passed on by fecal oral transmission. This can occur indirectly by drinking from contaminated lakes, streams, puddles, and shallow wells or directly from the ingestion of contaminated feces.
Symptoms of giardia include acute or chronic diarrhea and rarely more severe signs such as vomiting, dehydration or weight loss. Some pets may carry giardia and be asymptomatic.
Diagnosis is made by testing the stool of affected pets. Occasionally giardia can be found by evaluating a stool sample under the microscope. But more reliably, giardia can be diagnosed with a SNAP test that detects giardia antigen in the stool, even at small levels.
Treatment of giardia can depend on the severity of symptoms. Typical treatment is with metronidazole (an antibacterial, antidiarrheal medication) which is given for 5-10 days and/or fenbendazole (aka Panacur -a dewormer) which is given once daily for 3-5 days. Bland diets that are easily digested are often prescribed to expedite return to normal stools. If a pet has other symptoms such as dehydration, nausea, blood in the stool or other concerning symptoms other diagnostics or therapies may be warranted.
Environmental control is an important step in helping prevent reinfection or transmission of infection to other pets/humans. Giardia can persist for months in cold water or damp, cool environments. Chemical disinfectants such as bleach (diluted 1:32 with water) can be helpful in cleaning up kennels and areas that can be safely cleaned with bleach. Swimming pools are not often contaminated if they are properly chlorinated, as chlorine also destroys giardia. Picking up fecal material and allowing a yard to dry out in the sun is also an effective way of controlling giardia in the environment.
by Lodi Vet | Mar 10, 2017 | Dogs, Educational Materials, How To
It takes about 1-2 teaspoons of urine to run a urinalysis. Even obtaining that small amount may seem like a monumental task for some owners. To aid in this adventure, we have put together some suggestions to help make this process easier for you. Please feel free to contact us at any point with questions.
- Keep your dog on a leash while trying to obtain a sample. You may want to enlist help to catch the sample.
- If you dog squats very low to the ground, we recommend sliding a saucer, plate, or other shallow dish under your dog when they are ready to urinate (It is important to make sure the collection device is clean and dry). Once collected, transfer the urine to a sterile container for transporting.
- If your dog lifts his/her leg or squats high, you can use a “dipper” to catch the urine. A “dipper” can be made by taping a small disposable papercup to a handle (stick, dowel rod, ruler, etc.). This allows you to collect urine without reaching under your dog with your hand. A soup ladle works well! This method is effective for dogs that maybe shy to you reaching under them.
- If your dog is uncooroperative in any of these methods, please contact us. We can help. We can set up an appointment for a staff member to collect urine with you outside, or we can collect urine by cystocentesis. Cystocentesis is done by passing a needle into the bladder and obtaining a sample directly. Although this sounds unpleasant, it is surprising how well dogs tolerate the procedure. It is important to keep your dog away from their yard and grass for at least two hours prior to this appointment. When you arrive at the hospital for your appointment, please do not let them sniff around outside, but come directly inside from your vehicle.
After obtaining the sample, it is extremely important to get the sample to us in a reasonable amount of time. For best results, this sample should be processed within 2 hours after collection. If that is now possible, the sample should be refrigerated and tested within 6 hrs.
by Lodi Vet | Mar 9, 2017 | Dogs, Educational Materials
A malocclusion is the abnormal alignment of teeth. One particular type of malocclusion that can be seen in puppies is base narrow k9 teeth. This is when the k9 teeth on the lower jaw are too close together, or the lower jaw is too short causing the k9 to contact the upper jaw abnormally. In severe cases, these lower k9 teeth will puncture into the hard palate causing pain, damage and infection. For these severe cases, treatment will require extraction of the teeth causing trauma. In milder cases, in which no major damage is occurring, we can use ball therapy to attempt to correct the malocclusion as the puppy grows.
The concept of ball therapy is very simple. Dogs should be encouraged to carry an appropriate sized ball in the mouth just behind the canine teeth. The presence of the ball applies force to the canine teeth– essentially acting like a retainer, training the teeth into a more appropriate position. The ball should be a smooth rubber ball appropriately sized for the puppy – good examples include: rubber balls, Kong™ toys or road hockey balls. Your veterinarian can guide you on the appropriate sized ball for your puppy. Tennis balls should NOT be used as the outer covering is very abrasive and can cause dental wear.
Unfortunately, ball therapy will not prove to be effective for all puppies with malocclusions, but the risk is very low in attempting this method. Some puppies with malocclusions will require veterinary dental procedures to help correct their bites.
by Lodi Vet | Mar 9, 2017 | Dogs, Educational Materials
 Diabetes mellitus is a common problem in dogs. Caring for a diabetic animal requires some effort, but most pets remain happy and comfortable. Successful patient management requires a team effort between you and our veterinary care team.
Diabetes mellitus is a common problem in dogs. Caring for a diabetic animal requires some effort, but most pets remain happy and comfortable. Successful patient management requires a team effort between you and our veterinary care team.
What is diabetes mellitus?
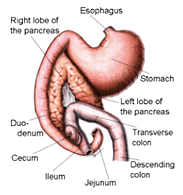
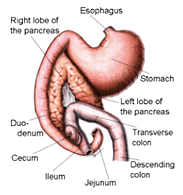
Diabetes mellitus is a disease caused by a deficiency of (or lack of response to) insulin. Insulin is a hormone that is produced by the pancreas. The cells of the body require blood sugar (glucose) for food and they depend on the bloodstream to bring glucose to them. The cells cannot, however, absorb and utilize glucose without insulin. Insulin is necessary for the movement of glucose from the blood into the cells of the body.
What are the signs of diabetes?
Excessive thirst, frequent urination, increased hunger, sudden weight loss and weakness are seen in dogs with diabetes. Without insulin, glucose remains in the bloodstream and eventually passes into the urine. This causes increased urination, which then leads to an increase in thirst. Hunger increases because the body cannot use the glucose in the blood, which results in the body destroying muscle and fat to use as energy sources. Elevated glucose levels can also lead to glucose accumulation within the lens of the eye, which can lead to the formation of cataracts. If left untreated, this disease sets off a series of events which results in weight loss, major organ system failure, blindness, and eventually coma and death.
Why is my dog diabetic?
Dogs become diabetic due to genetic factors, combined with environmental triggers. Many dogs with diabetes are overweight, or were previously, and this may play a role.
Is there a cure for diabetes?
Unfortunately, the answer is no. With very rare exceptions, diabetes in dogs is a permanent condition and life-long therapy is necessary.
Will my dog need insulin?
Yes. Most diabetic dogs are insulin dependent, which means that they need regular insulin injections to control glucose levels.
What does the insulin do?
Insulin moves glucose from the blood into the cells. Glucose is an essential fuel for most of the tissues in the body, and without insulin, cell metabolism is severely compromised. Providing insulin in the form of an injection allows your dog to be able to utilize its glucose and maintain relatively normal glucose levels.
How do I give insulin?
Our veterinary team with show you exactly how to give insulin injections, but it’s really very simple. The insulin dose is pulled up into a special syringe, and injected under the skin. It is often easiest to inject between the shoulder blades or along the neck.
Do the insulin injections hurt?
Insulin syringes have very small needles, and most dogs do not notice the injection. It is often easiest to administer the injection while your dog is distracted with food, a treat, or a toy. Most people are surprised at how easy insulin injections are to give.
How do I dispose of my used supply of needles and syringes?
Used needles and syringes need to be properly disposed of for both your safety and ours. You will be required to purchase a “SHARPS” container for a fee. This fee covers the container purchase, plus the proper disposal of the used/full container.
We will not accept used needles and syringes that are stored in containers other than the approved “SHARPS” container. Once the “SHARPS” container is full, simply return it to our office. We will dispose of it and you can purchase a replacement container.
What follow-up is involved with treating diabetes in dogs?
In the non-diabetic dog, adequate amounts of insulin are produced continually (or as needed) by the pancreas to maintain normal blood sugar levels. When we give insulin injections, we administer a fixed amount at one time and that insulin is slowly released over several hours. A blood glucose curve is needed to determine how fast the injected insulin gets into the bloodstream over several hours. Based on these results, we can determine if the correct type of insulin is being used and if the dose needs to be adjusted. Blood glucose curves are needed periodically to insure that the proper amount of insulin is being used. Blood glucose curves are performed by obtaining a blood glucose level every 2 hours over a 12 hour period. Generally, if your dog’s blood glucose is elevated throughout the curve, their insulin dose needs to be increased. If your dog’s blood glucose level is too low throughout or at any point during the curve, the insulin dose needs to be decreased.
What are the possible complications associated with treating my dog with insulin?
The most serious complication involved in treatment of diabetes is administration of too much insulin, which can trigger a dramatic drop in blood sugar leading to weakness, nausea, incoordination, seizures, and even death. Immediate feeding of a sugary food (honey, syrup, etc.) usually helps reverse this reaction. Other difficulties encountered generally revolve around finding the correct amount, timing, and type of insulin given. While this not often the case, “problem diabetes” do exist and have a higher incidence of concurrent disease such as lower urinary tract infections, kidney disease and liver disease.
Can I monitor my dog’s blood sugar (glucose) at home?
Learning to measure your dog’s glucose levels is very worthwhile. Firstly, information collected at home is a reflection of what’s happening day-to-day in your dog’s normal living environment. Home glucose monitoring would allow you to be able to perform your dog’s glucose curves at home. Our veterinary team can use the values you obtain at home to adjust insulin therapy more appropriately and accurately. Secondly, if your dog seems unwell, you can quickly determine if blood sugar levels are dangerously low or high. It is very important to always consult our veterinary team prior to making any insulin adjustments.
What are the costs associated with treating my diabetic dog?
The major costs associated with treatment of diabetes include insulin, syringes, and the cost of the glucose curves to regulate insulin requirements. We can give you a more accurate estimation of treatment cost at your consultation appointment.
Making the decision to care for your dog with diabetes is a big commitment, but many owners of diabetic dogs have found treatment to be a very rewarding and enriching experience. There is a lot to learn and it is important to be patient with yourself and your dog during the learning process. Diabetes is a serious disease, but it can usually be well-controlled, enabling your pet to lead a happy and comfortable life.
Our veterinary care team has reviewed the following websites on canine diabetes and found them to be an accurate source of valuable information:
www.veterinarypartner.com
www.alphatrakmeter.com
by Lodi Vet | Mar 9, 2017 | Cats, Dogs, Educational Materials
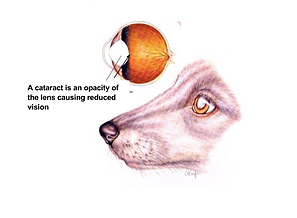
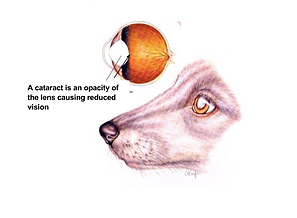 A cataract is an opacity (cloudy area) within the lens of the eye. Cataract size can range from small to large. Small cataracts minimally alter vision, whereas larger cataracts can result in blindness.
A cataract is an opacity (cloudy area) within the lens of the eye. Cataract size can range from small to large. Small cataracts minimally alter vision, whereas larger cataracts can result in blindness.
Cataracts are very common and can occur for a variety of reasons, including:
- Congenital (born with cataracts)
- Genetic (born with predisposition to form cataracts)
- Age related
- Diabetes
- Trauma
- Dietary deficiencies
Although cataracts are considered benign, there are still concerns or complications that can arise as a result of a pet having cataracts. These include:
- Decreased vision/blindness
- Lens luxation (lens can become loose in the eye causing damage)
- Uveitis (inflammation of the inner eye)
- Glaucoma (occurs secondary to inflammation)
Treatment of cataracts is not always warranted. If the cataract is small and uncomplicated, no treatment is needed. Treatment is warranted if a cataract causes blindness, luxates, or if it results in inflammation or glaucoma of the eye. Treatment options include:
- Minor episodes of inflammation of the eye secondary to cataracts can be treated with prescription anti-inflammatory eye drops.
- Surgical removal of cataract with or without artificial lens placement
- Phacoemulsification (breaking apart the lens with sound waves)
- Enucleation (removal of the entire eye) may be needed in cases with glaucoma
- Although there are over the counter eye drops claiming to “treat” or “cure” cataracts these products DO NOT WORK
by Lodi Vet | Mar 9, 2017 | Dogs, Educational Materials
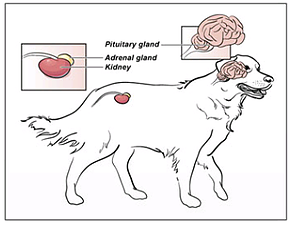
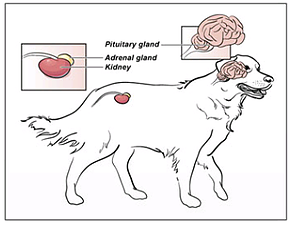 The adrenal glands are a pair of small glands located just in front of the kidneys. They make cortisol (a corticosteroid hormone), which helps the body adapt to stress. Cortisol helps the body prepare for a “fight or flight response” by preparing the body’s resources (such as fat, sugar, and water stores) for rapid breakdown in a stressful situation. However, long-term excesses of cortisol are harmful to your pet. Too much production of cortisol is called “Cushing’s disease” or hyperadrenocorticism. The opposite of this endocrine disorder is called hypoadrenocorticism or Addison’s disease, a condition that results in too little cortisol production from the adrenal glands.
The adrenal glands are a pair of small glands located just in front of the kidneys. They make cortisol (a corticosteroid hormone), which helps the body adapt to stress. Cortisol helps the body prepare for a “fight or flight response” by preparing the body’s resources (such as fat, sugar, and water stores) for rapid breakdown in a stressful situation. However, long-term excesses of cortisol are harmful to your pet. Too much production of cortisol is called “Cushing’s disease” or hyperadrenocorticism. The opposite of this endocrine disorder is called hypoadrenocorticism or Addison’s disease, a condition that results in too little cortisol production from the adrenal glands.
Types of Cushing’s Disease:
PDH (Pituitary Dependent Hyperadrenocorticism (85% of cases): PDH is caused by the pituitary gland in the brain sending too much signal for the adrenal glands to produce cortisol. This is a benign, yet functional tumor of the pituitary gland.
Adrenal Tumors (15 % of cases): Adrenal tumors can cause too much cortisol production, and can be benign or malignant.
Symptoms of Cushing’s Disease:
Many times the symptoms progress gradually and can be mistaken for the normal aging process. Animals may not have all of these symptoms.
- Drinking excessively, urinating excessively, urinary incontinence
- Increased appetite
- Pot-bellied appearance
- Muscle weakness (lethargy, reluctance to jump)
- Skin Disease
- Hair loss on body (not head or limbs)
- Thin skin, poor wound healing
- Hair not growing back after clipping
- Darkening of skin
- Persistent or recurrent skin infection
- Excessive panting
�Testing for Cushing’s Disease:
Medical Workup (chemistry panel, complete blood count, and urinalysis with bacterial culture): we can be suspicious of Cushing’s disease based on the results of this workup.
LDDS (Low Dose Dexamethasone Suppression Test): the most common screening test for Cushing’s disease.
- Blood samples are drawn right after a small dose of Dexamethasone is administered, then again at 4 hours and 8 hours later.
- The pet stays in the hospital for the day (9 hours) for this test.
- This test cannot be done at the same time as a surgery, sedation, or general anesthesia.
ACTH Stimulation Test: usually done to monitor effectiveness of treatment.
- Blood sample is drawn initially, then one hour after the administration of ACTH.
- The pet needs to stay in the hospital for about 2 hours.
Abdominal ultrasound: used to assess adrenal glands for abnormalities- this can be done during the hospital stay for the LLDS test.
Treatment:
Most often, treatment for Cushing’s disease involves giving an oral medication indefinitely. However, Cushing’s disease caused by an adrenal tumor is usually treated with surgical removal of the tumor.
Trilostane
Trilostane is an inhibitor of an enzyme involved in the production of several steroids made in the body, including cortisol. Inhibiting this enzyme decreases the production of cortisol.
- Trilostane is given once or twice a day with food.
- Common side effects are mild lethargy and appetite reduction especially when medication is started and the body adapts to its hormonal changes.
- Addisonian reactions have been reported in which the adrenal cortex dies off. Most reactions are minor and can be reversed with discontinuation of trilostane; however, permanent Addisonian reactions are rare, just as with Lysodren. In two studies, the risk of a permanent or life-threatening Addisonian reaction was 2-3% with trilostane and 2-5% with Lysodren.
- ACTH stimulation testing needs to be performed 10, 30 and 90 days after start of treatment and 30 days after each dose adjustment- always 4-6 hours post pill.
Mitotane
- Mitotane (Lysodren) is a drug used to treat Cushing’s disease because it actually destroys some of the cells of the adrenal gland to reduce the amount of cortisol produced. Every animal responds differently to the drug, so careful monitoring is necessary to determine the right dose for each pet. The treatment starts with induction, and then a maintenance dose is usually given for the rest of the pet’s life.
- Induction: Mitotane is given orally at home for approximately 7-10 days, or until signs of lower cortisol levels develop. Then an ACTH Stimulation test is performed to evaluate the adrenal function.
- Maintenance: If the ACTH stimulation test shows that enough Mitotane has been given, a maintenance dose is started (usually given twice a week).